What Is Diabetes Mellitus?
Diabetes mellitus is a term used to describe a group of metabolic disorders characterized by persistently high blood sugar levels. This causes various issues and if left untreated, can cause many complications. Diabetes can occur when the pancreas is not producing adequate insulin or if there is insulin resistance.
Diabetes can be divided into type 1 diabetes, type 2 diabetes, and gestational diabetes. In 2017, the estimated global economic cost of diabetes related issues was US$727 billion. In the United States in 2012, diabetes cost almost US$245 billion. Diabetics have medical expenditure that is on average 2.3 times higher.
1. Types
Type 1 diabetes mellitus (T1DM) occurs due to the failure of the pancreas to produce adequate insulin because of the loss of beta cells in the pancreas. T1DM was previously known as juvenile diabetes as it generally begins in the younger population. The beta cells are lost due to an autoimmune response. Type 2 diabetes mellitus (T2DM) is due to insulin resistance and is previously known as adult-onset diabetes.
However, since it is increasingly common among the pediatric population due to high obesity rates, this term is now rarely used. T2DM is the commonest type of diabetes. Gestational diabetes occurs when a pregnant woman without a history of diabetes develops high levels of blood sugar during pregnancy.
2. Etiology and Risk Factors
T2DM has been thought to be due to a combination of genetic and environmental factors where those with susceptible genes lead a sedentary lifestyle and have excessive intake of calories. It is estimated that about 90% of patients with T2DM are obese. Genetic studies have found that there are many genetic variants that increases the risk of T2DM such as the transcription factor 7-like 2 (TCF7L2) gene.
Risk factors of T2DM are obesity, positive family history, age of more than 45 years old, race (of Native American, Asian American, Pacific Islander, African American, or Hispanic descent), hypertension, high cholesterol, history of gestational diabetes, polycystic ovarian syndrome, history of impaired fasting glucose or impaired glucose tolerance, schizophrenia, preeclampsia, and depression.

3. Epidemiology
Based on a report by the Centers for Disease Control and Prevention (CDC) in 2017, it is estimated that 94% of the population (30.3 million individuals) as of 2015 had diabetes while an additional 84.1 million adults had prediabetes. In non-Western countries where the diet contains fewer calories and higher caloric expenditure, T2DM is less common. However, these numbers are increasing as more people adopt Western lifestyles.
The International Diabetes Federation has predicted that from 2011 to 2030, the number of diabetics will increase from 366 million to 552 million. The top 10 countries with the most number of diabetics are India, China, United States, Indonesia, Japan, Pakistan, Russia, Brazil, Italy, and Bangladesh.

4. Signs and Symptoms
The signs and symptoms of diabetes are unintentional weight loss (with Type I Diabetes), increased urination (polyuria), increased hunger (polyphagia), fatigue, blurry vision, nausea, vomiting, abdominal pain, and increased thirst (polydipsia).
In type 1 diabetes, symptoms can begin and develop rapidly while it may be slower in individuals with type 2 diabetes. Patients with diabetes also tend to heal more slowly and may experience pruritus (itchy skin), prone to skin infections (yeast), vision changes, skin rashes, and a smell of acetone from their breath. Depending on the type of diabetes, some symptoms may be more common compared to another type. Some symptoms may also be more acute while some only occur as the disease has progressed several years later.

5. Assessment
It is important for healthcare providers to ask about the duration of the diabetes and the care they receive as complications of diabetes are generally related to the duration the patient has had the disease. Disease control is also important as those with poorly controlled diabetes are more likely to develop complications and infections.
Assessment of hypoglycemic reactions are also important so the patient is properly educated to look out for symptoms of diabetic ketoacidosis and other emergencies. Patients should be assessed for visual issues, neuropathy, renal function, hypertension, and recent symptoms of both hyper and hypoglycemia. Immunization history is also important as vaccinations can help decease the risk of infections among diabetics.

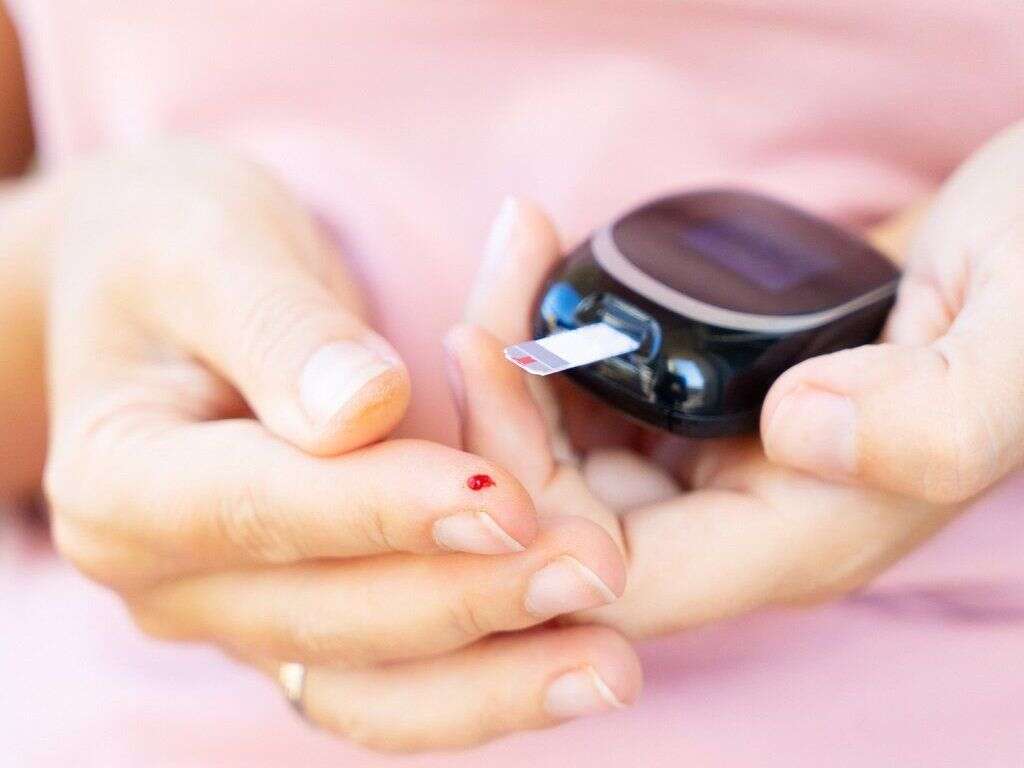
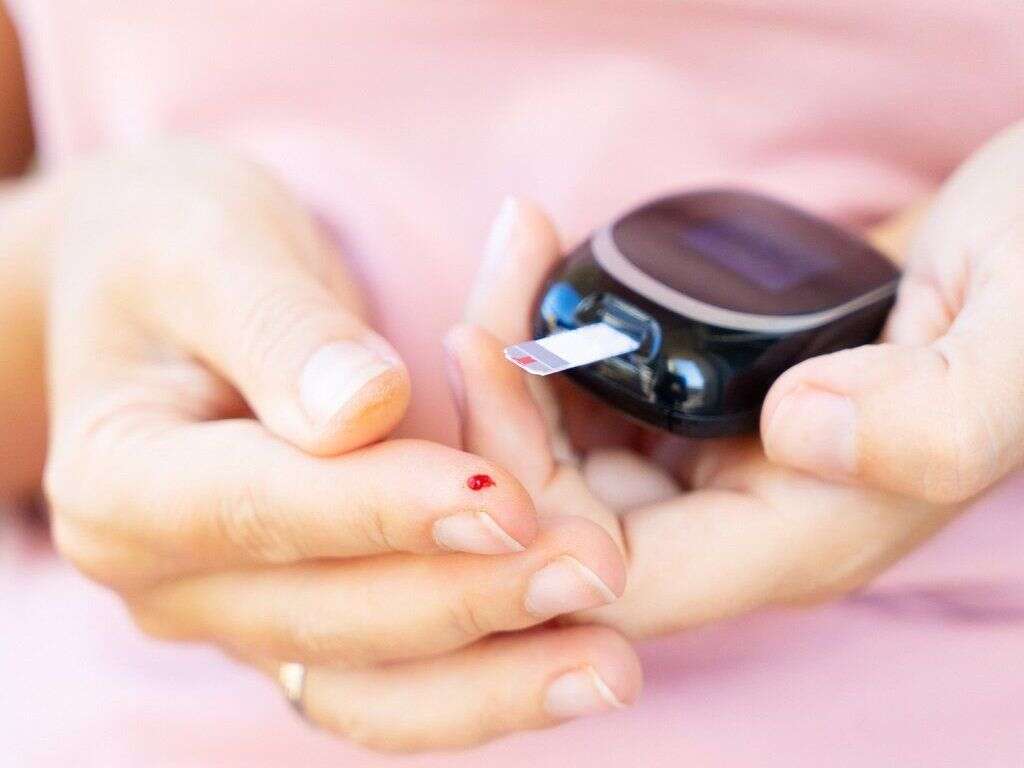
6. Diagnosis
The criteria for the diagnosis of diabetes per the American Diabetes Association are any of the following: A fasting plasma glucose of 7.0 mmol/L or higher, 2-hour plasma glucose level of 11.1 mmol/L or higher, HbA1c level of 6.5% or higher, or a random plasma glucose level of 11.1 mmol/L or higher in those with symptoms of hyperglycemia. Repetition of the test can be performed for confirmation purposes (on a different day).
Confirmation can also be achieved when the results of 2 different tests are above the threshold for diagnosis. Those with levels higher than normal but below the criteria to be diagnosed with diabetes are considered to have impaired fasting glucose or impaired glucose tolerance.

7. Treatment and Management
The management of diabetes aims to control the blood glucose level and maintain it at a normal level. Besides having a healthy diet, losing weight, exercise, and quitting tobacco products, medications such as metformin, insulin, and glucagon-like peptide 1 (GLP1) agonists can also be used. Since cardiovascular disease is a known complication for diabetics, their blood pressure should be maintained below 130/80 mmHg.
This can be done using angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), calcium channel blockers (CCBs), and more. For those who are obese, weight loss surgery may also be beneficial. A kidney transplant or dialysis may be required for those with end-stage renal disease. Regular follow-ups with a podiatrist, nephrologist, and ophthalmologist should also be required.

8. Prevention
For T1DM, there is no known preventive measure. However, for T2DM, which accounts for 85% to 90% of all cases, the disease can be prevented or delayed by maintaining a normal body weight, having a healthy diet, and having a regular exercise routine. The American Diabetes Association recommends sedentary activities last no more than 90 minutes at a time.
Dietary changes such as having a diet rich in fiber, whole grains, good fats, and limiting the consumption of sugary beverages and red meat can also be beneficial. The use of tobacco has also been found to increase the risk of diabetes. Some studies have also shown the use of medications such as valsartan, metformin, and rosiglitazone may help delay progression to diabetes. However, lifestyle interventions are generally more effective than medications.

9. Prognosis
The prognosis of diabetes mellitus is greatly dependent on the control of the disease. When there is poor control, this means that there is a prolonged duration where there is elevated blood glucose. This results in various complications such as retinopathy, neuropathy, and nephropathy.
Various studies have found that those who are intensively treated have been shown to have a significantly lower rate of disease progression. This means that there should be tight glycemic control with a HbA1c level of less than 7%. Based on these studies, not only does this decrease both the risks of microvascular and macrovascular disease, patients managed this way also had a longer life expectancy. In 2015, diabetes was reported to be the 7th leading cause of death in the United States. It is a major cause of blindness, leading contributor to end-stage renal disease, leading cause of nontraumatic lower limb amputations, and increases the risk of cardiovascular disease, cancer, and pneumonia.

10. Patient Education
Patients should not only be educated through pamphlets and brief instructions as patient education is crucial for patients with diabetes. Diabetics require efforts from their physician, nutritionist, and other health professionals. Educating diabetics is a lifelong exercise and cannot be accomplished through 1 or 2 sessions.
Studies have found that those with poorly controlled diabetes benefit more from individual education as it helps them achieve better compliance and self management. Education should include nutrition, exercise, foot care, compliance to medication, and the importance of regular check-ups with various physicians (for eyes, kidneys, feet). Diabetes education is beneficial for all patients at all stages of the disease.












