What Is Cradle Cap?
 Article Sources
Article Sources
- 1. 'Cradle Cap: What It Is, Symptoms & Treatment.' Cleveland Clinic, my.clevelandclinic.org/health/diseases/15786-cradle-cap-seborrheic-dermatitis-in-infants.
- 2. 'Cradle Cap (Seborrheic Dermatitis) in Infants (for Parents) - Nemours KidsHealth.' Edited by Mary L. Gavin, KidsHealth, The Nemours Foundation, Feb. 2019, kidshealth.org/en/parents/cradle-cap.html.
- 3. 'Cradle Cap.' Seattle Children's Hospital, www.seattlechildrens.org/conditions/a-z/cradle-cap/.
- 4. 'Seborrheic Dermatitis (Cradle Cap).' Symptoms, Causes and Treatment, www.nationwidechildrens.org/conditions/cradle-cap.
- 5. 'Seborrheic Dermatitis (Cradle Cap).' Johns Hopkins Medicine, www.hopkinsmedicine.org/health/conditions-and-diseases/seborrheic-dermatitis-cradle-cap.
- 6. 'Cradle Cap.' Mayo Clinic, Mayo Foundation for Medical Education and Research, 27 Oct. 2020, www.mayoclinic.org/diseases-conditions/cradle-cap/diagnosis-treatment/drc-20350400.
Cradle cap can give new parents a scare. This common skin condition typically occurs during a newborn’s first three months of age, affecting seven out of 10 babies. Cradle cap is harmless and often treatable with self-care solutions at home. Also known as seborrheic dermatitis, the term, cradle cap, is used when the rash affects the scalp.1‘Cradle Cap: What It Is, Symptoms & Treatment.’ Cleveland Clinic, my.clevelandclinic.org/health/diseases/15786-cradle-cap-seborrheic-dermatitis-in-infants.
Although it’s unpleasant to look at, cradle cap isn’t painful for your baby and shouldn’t cause them any discomfort, including itching. Most cases go away on their own without care, but some symptoms may require a physician’s visit.

1. Symptoms of Cradle Cap
Parents often notice cradle cap quickly. It develops on the infant’s head between the ages of two weeks and twelve months, but it’s most common from two weeks to six weeks. Cradle cap starts in patches and may cover the entire scalp. It’s red and scaly in appearance with crusty yellow patches. The rash may have greasy patches and can flake.
Seborrheic dermatitis can also appear in the skin folds as a bright red rash. Common areas include under the arms, behind the knees, in the elbow crease, and the neck and groin fold.2‘Cradle Cap (Seborrheic Dermatitis) in Infants (for Parents) - Nemours KidsHealth.’ Edited by Mary L. Gavin, KidsHealth, The Nemours Foundation, Feb. 2019, kidshealth.org/en/parents/cradle-cap.html.

2. Cradle Cap Causes
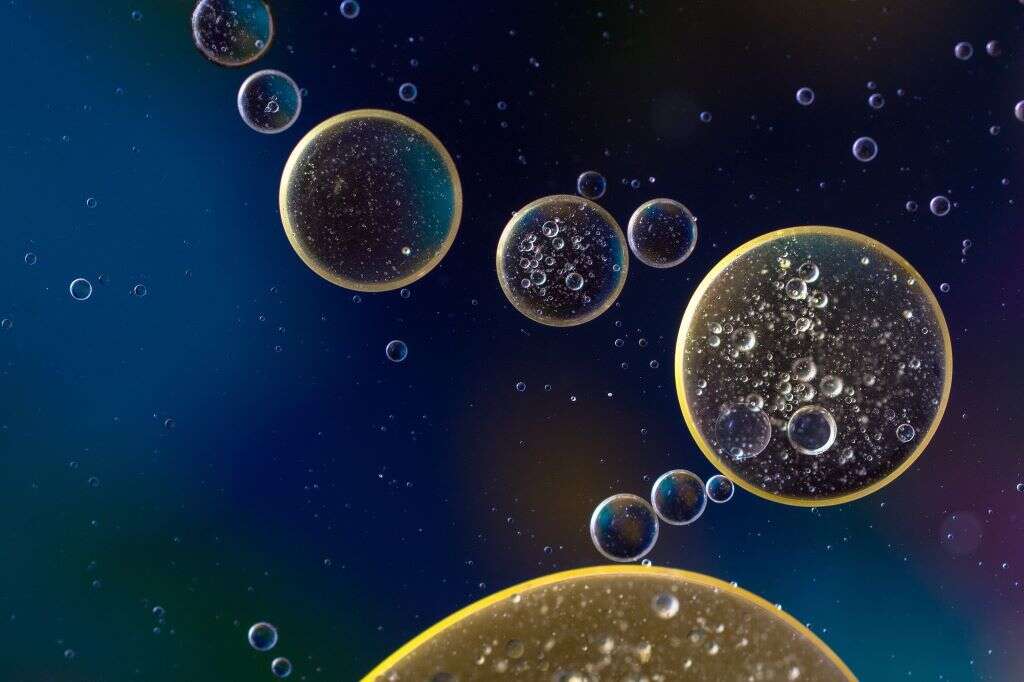
Medical professionals don’t know the exact reason cradle cap occurs. Experts speculate the skin condition happens when there is an overproduction of sebum oil by the sebaceous glands. This excess oil may mix with a type of yeast found on the surface of the newborn’s skin.
Before birth, the mother’s hormones traveled freely through the placenta into the fetus.3‘Cradle Cap.’ Seattle Children’s Hospital, www.seattlechildrens.org/conditions/a-z/cradle-cap/. These hormones may be responsible for the overproduction of sebum oil after birth. The good news is it’s not contagious, usually resolves itself, and rarely causes babies discomfort.
3. Home Treatments for Cradle Cap
In most cases, cradle cap resolves on its own, but several options are available for home treatment. These methods may help cradle cap go away faster and reduce some new parent anxiety. Since the crust may be hard to remove on its own, soften it with petroleum jelly or baby oil before bath time.
Wash your baby’s hair regularly, using a soft-bristled brush, rough washcloth or your fingers to massage the top of their head. Continue for up to five minutes. These steps can help loosen the flaky area faster.

4. When Should You Call the Doctor?
If your child’s cradle cap isn’t improving or appears to be worsening, you may want to call your pediatrician. Another situation that requires a doctor’s advice is when the rash spreads.4‘Seborrheic Dermatitis (Cradle Cap).’ Symptoms, Causes and Treatment, www.nationwidechildrens.org/conditions/cradle-cap.
Although cradle cap is common on the scalp, you want to prevent it from spreading and affecting larger areas of the body. When it involves the skin folds, there’s more of a chance of developing an infection. Your physician may want to prescribe a treatment to help clear it up faster.

5. Diagnosing Cradle Cap
Fortunately, when you take your baby to the pediatrician for cradle cap, the diagnosis is easy. You won’t have to worry about invasive tests upsetting them.
Instead, your physician will make observations based on the rash. They’ll also verify the infant is in good health, and the only problem is the yellowish, flaky skin.5‘Seborrheic Dermatitis (Cradle Cap).’ Johns Hopkins Medicine, www.hopkinsmedicine.org/health/conditions-and-diseases/seborrheic-dermatitis-cradle-cap. They may prescribe a treatment to reduce the skin condition quicker than home treatment and possibly schedule a follow-up appointment in a few weeks to check the progress.

6. Medical Solutions for Cradle Cap
After confirming the diagnosis, your doctor might prescribe a special shampoo. The most common formula contains 2 percent antifungal ketoconazole. Avoid getting the shampoo in your baby’s eyes. Your doctor may also suggest a low-potency corticosteroid cream or lotion for a short duration to speed-up the healing process for persistent rashes
Always avoid using any over-the-counter products not intended for infants without consulting your pediatrician first. Special shampoos for adults can be toxic to children.6‘Cradle Cap.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 27 Oct. 2020, www.mayoclinic.org/diseases-conditions/cradle-cap/diagnosis-treatment/drc-20350400.

7. How Long Does the Treatment Take?
The duration of treatment for cradle cap depends on the severity of the rash. Some cases can clear up in a few weeks with little to no extra care by parents.
While cradle cap may be unsightly, it’s important to remember that the condition isn’t itchy or painful to your child. Most instances of cradle cap go away on their own by keeping the scalp and hair clean. Few cases of the flaky, yellow rash stick around past your child’s first birthday or return after a year has passed.

8. Cradle Cap Can Come Back
It’s not uncommon for cradle cap to go away and reappear a few weeks or months later. It would be best if you treated these recurrences the same as the initial outbreak. Keep an eye on the rash. Keep the area clean. Call your pediatrician if spreading to other skin areas occurs.
Continue to follow the gentle washing and scalp brushing. These simple steps can not only help get rid of cradle cap but prevent it from coming back after it’s resolved.

9. Preventing Cradle Cap
There’s not much parents and caregivers can do to prevent cradle cap from developing. Experts believe that hormonal changes that pass from the mother to her baby before birth may cause too much sebum in the glands and hair follicles. Additionally, a yeast called Malassezia that grows in the sebum along with bacteria may play a role in developing cradle cap.6‘Cradle Cap.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 27 Oct. 2020, www.mayoclinic.org/diseases-conditions/cradle-cap/diagnosis-treatment/drc-20350400.
The most important steps you can take are keeping your baby clean, washing their hair regularly, and checking their scalp and body for new rashes. Also, make regular appointments with your pediatrician to ensure your child is healthy and meeting all their developmental milestones.

10. Complications of Cradle Cap
Although cradle cap is common, there are a few potential complications. Along with the rash spreading to other areas of the body, infections can develop, leading to serious issues requiring immediate medical attention. Signs include red skin, blisters, and areas that are warm to the touch.
Other symptoms may include a swollen appearance and pus from the blisters. Unlike the standard cradle cap, when an infection develops, it might become painful for your child. These developments may require antibiotics to clear up the infection.