What Is Colitis?
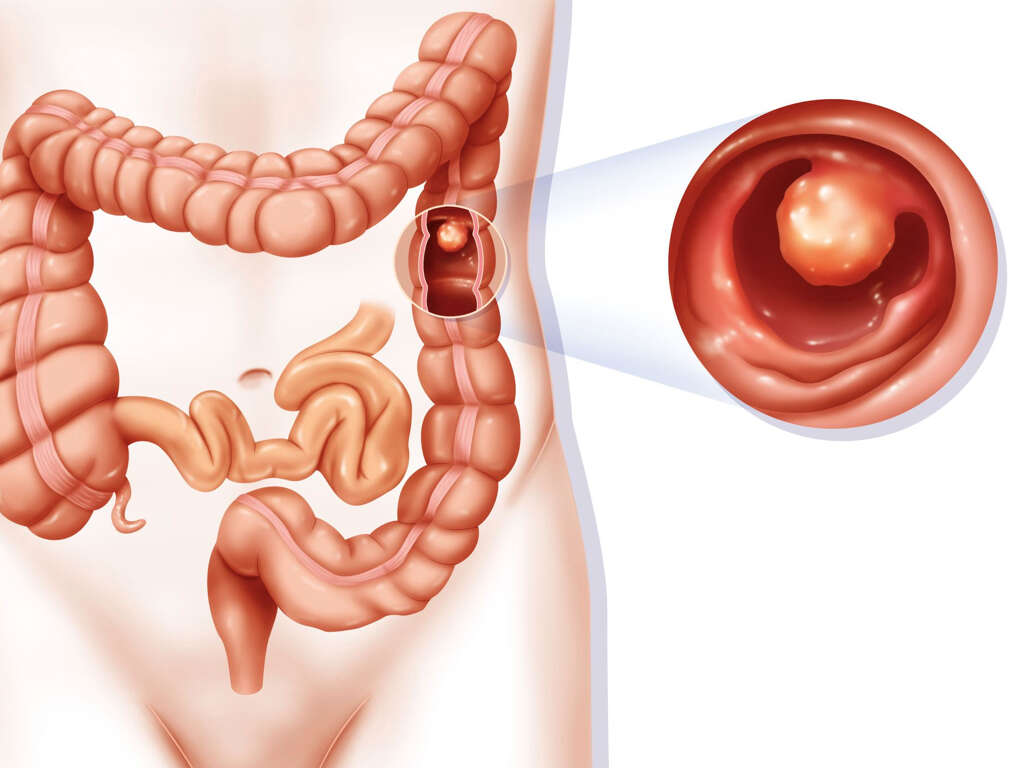
In simple terms, colitis is the inflammation of the colon. The condition is usually associated with the inflammation of the small intestines called enteritis, proctitis or inflammation of the rectum, inflammatory bowel disease (IBD), decreased blood supply to the colon, and invasion of the wall of the colon by lymphocytes.
Colitis affects the inner lining of the colon. There are different types of the condition, which include ulcerative colitis, Crohns colitis, diversion colitis, ischemic colitis, infectious colitis, fulminant colitis, collagenous colitis, chemical colitis, microscopic colitis, lymphocytic colitis, and atypical colitis. Colitis can lead to a medical emergency especially if the colon is severely damaged.

1. Symptoms of Colitis
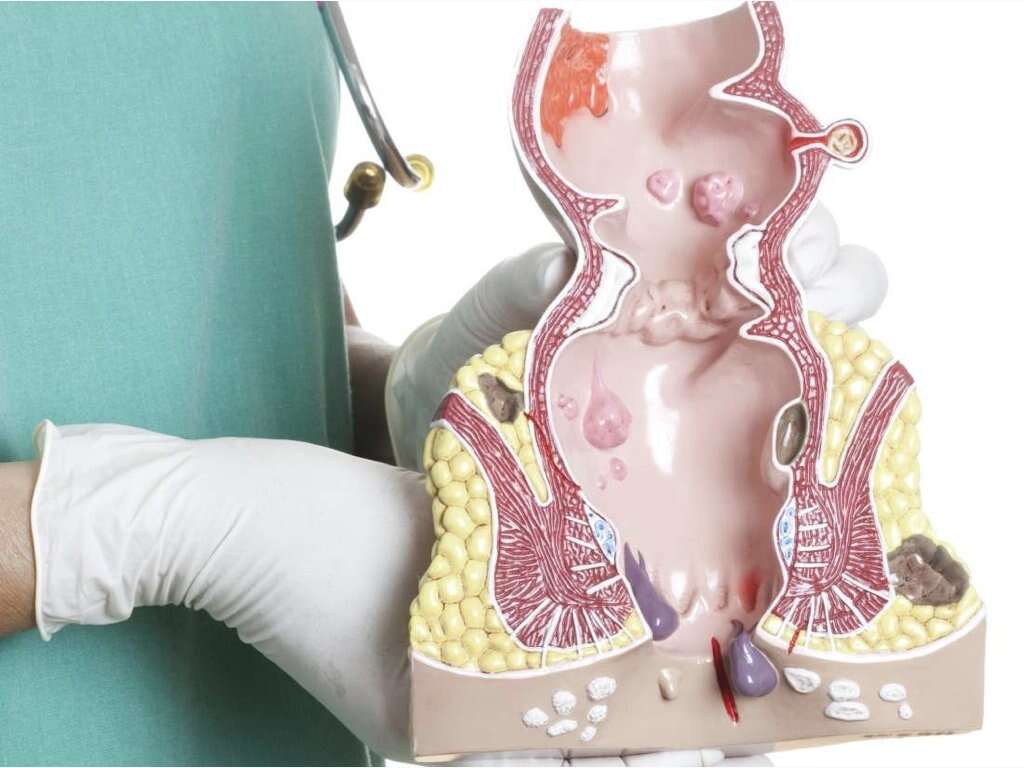
Chronic diarrhea is the most common symptom of all types of colitis. Most of the patients complain of the urge to go to the bathroom as a result of constant bowel movement. The resultant constant irritation of the rectum leads to small bulges, a condition called diverticula. Additionally, people with colitis usually pass stools in very small amounts.
Other symptoms also include loss of weight, dehydration, fever, abdominal pain, rectal problems, chronic constipation, and bloody stool. Blood in stools means that the colon is severely damaged. This is a dangerous sign that should be treated as a medical emergency.

2. Causes of Colitis
The specific cause of colitis is not known. However, there are many risk factors and theories explaining why the condition occurs.
According to some of the theories, colitis is an autoimmune condition targeting the gastrointestinal tract. There are also a number of known risk factors for colitis. These include long medical history of infections and antibiotic use and abuse.

3. Family History
A family history of colitis, and other GIT problems, living in poor conditions, or far from the equator are also causative factors for colitis.
However, these risk factors do not mean that the person who has any of them will definitely develop colitis. Only that they increase the risk of developing colitis.
4. Colitis and Chronic Diseases
Colitis is itself a chronic disease that can be confused for other chronic conditions, especially Crohn’s disease. However, while Crohn’s disease affects any part of the GI tract, colitis only affects the rectum or large intestines.
Any chronic inflammatory disease can cause severe damage to the inner lining of the large intestine, but each case presents differently. And while colitis may have causative factors like parasites, viruses, and bacteria, it is also associated with bad habits such as smoking. Amoeba infestation and Giardiasis may also be confused with colitis.

5. Complications of Colitis
There are many complications of colitis which can include toxic megacolon and chronic anemia. Toxic megacolon is when a portion of the colon becomes dilated and there is wide spread toxicity.
The symptoms of megacolon include chronic abdominal pain, fever, diarrhea, malnutrition, and dehydration. The most serious complication of the mega colon is a ruptured colon. Anemia is also a common complication of colitis that occurs due to the constant loss of blood.

6. Disease Process
There are many types of colitis, each of which presents in a different way. Ulcerative colitis generally develops when the immune system reacts to bacteria and substances in the gastrointestinal tract in an abnormal way. Additionally, medications such as antibiotics can destroy both healthy and unhealthy bacteria, which sets ground for other bacteria and other harmful microorganisms to release toxins that cause inflammations.
Ischemic colitis occurs when blood supply to the large intestines stops or slows as a result of blood clots or atherosclerosis. Microscopic colitis occurs when lymphocytes, a certain type of white blood cell, invade the colon tissue. Other types of colitis such as allergic colitis usually occur in infants.

7. Can Diet or Lifestyle Changes Ease Colitis?
It is important to make a few lifestyle changes in order to manage your colitis. Some natural practices can help ease some of the effects of colitis. For instance, intake of probiotics increases the numbers of beneficial microorganisms in the gastrointestinal tract, which can help reduce the symptoms of colitis.
Acupuncture, intake of wheatgrass, increased intake of omega-3 fatty acids, fiber, turmeric, folate, and folate-rich foods may also help. Additionally, regular intake of fiber-rich foods and reduction of refined carbohydrates can help improve the health of the colon.

8. Diagnosis
Upon visiting a physician, the patient will be asked about when the symptoms first appeared, and their frequency. This will be followed by a physical exam along with tests such as colonoscopy to view the inner aspect of the colon and rectum, and sigmoidoscopy to view the lower part of the colon and rectum.
Stool samples are also examined for color, consistency, and content. Abdominal imaging such as CT, MRI, and ultrasound are also used to determine the extent of the condition. A barium enema test may also be carried out to get a clear picture of the condition of the colon.

9. Treatment
The treatment of colitis depends on many factors such as the age of the patient, medical history, type of colitis, complications, and overall physical condition. The first and most important step in colitis treatment is bowel rest. It is recommended to eat and drink only what can be useful to your bowel, especially in cases of ulcerative colitis. You should also increase your fluid intake significantly and eat nutritious foods. Food supplements or intravenous supplements can also be considered to rest the colon as long as possible. Of course, it is better to quit smoking too.
Antibiotics are usually only prescribed in cases of some infections. Antispasmodic drugs are also recommended to relieve pain. If the medical treatment does not work, surgical treatment may be considered. Surgery involves the removal of part of, or the whole colon and/or rectum.

10. Long-Term Outlook
The long-term outlook for colitis differs according to many factors such as the type of colitis, age, and overall physical condition. Ulcerative colitis usually requires long-term treatment and possibly surgery. Other types of colitis may improve following medication without the need of performing any kind of surgeries. Early discovery of the condition, along with proper diagnosis, is critical for developing the best treatment plan for the condition. Besides, most of the complications can be prevented with early diagnosis. It helps to share with your doctor all the symptoms you have experienced.
In general, colitis is treatable, and some people even manage the condition with diet and lifestyle changes alone.