What Is Angioedema?
Angioedema is a swelling under the skin, often around the eyes, mouth, cheeks or lips that results in puffiness, welts, pain, unusual warmth, redness or discoloration. This swelling may come about from exposure to either a single environmental stressor or several. When experiencing angioedema, the most important thing is to stay calm, ask for help, and identify your symptoms so you can explain them to a loved one or medical professional.
Examples of angioedema exposure triggers include bee pollen, animal dander, prescription drugs, insect or snake bites, latex or food allergens. The severity of the onset can result from existing, known risk factors, or the symptoms may appear quite suddenly. Read more to learn about the causes of angioedema, its comparison to hives, risk factors, treatment options and when to seek medical care.

1. What Causes Angioedema?
Angioedema may be inherited from parent to child or may be triggered by environmental factors. The immediate cause is usually exposure to foreign substances, certain foods or medications. Acute onset of angioedema may come about due to a change in the seasons, such as a high pollen count during the beginning of spring. A patient may also experience angioedema as a result of common nutritional intolerances such as shellfish, peanuts, dairy, gluten or soy.
Another cause may be that your immune system is operating in a hypervigilant state to get rid of a toxin. This means that your immune system is working, but perhaps is working too well, causing you discomfort. Individuals for whom the immune system is already compromised due to another chronic health condition should not use immunosuppressants. Rely on what your doctor advises.

2. Is Angioedema the Same as Hives?
While “breaking out in hives” (urticaria) describes the experience of skin discoloration, swelling, puffiness, rashes or heat on the skin’s outer layer in response to an allergen, angioedema occurs at the skin’s deeper layers. Whereas hives appear on the top layer of skin (epidermis), angioedema affects the inner dermal and subcutaneous layers and may appear within the lips, throat and mouth at the mucosa layer (mucus membrane) or submucosal layers of tissue.
Angioedema therefore may be less visible to your loved ones and observers, but more painful for you. You may actually feel the swelling inside your mouth, throat or nose before it becomes visible to the naked eye. Even if you cannot externally see the rash or discoloration right away, go ahead and try some of the solutions seen here, or seek medical treatment to reduce the impact of the angioedema.

3. How Long Does Angioedema Last?
Angioedema usually clears up within 24 to 48 hours of its first appearance, even without prophylactic treatment. There is usually no scarring or permanent discoloration after the reaction has subsided. The condition can become serious, however, if the swelling results in closure of the nasal passageways or throat cavity. Having antihistamines on hand can significantly reduce the impact and duration of these episodes.
Some patients may experience recurring angioedema, or display chronic symptoms. In these cases, consider consulting a certified allergist or an ear, nose and throat specialist (otolaryngologist) who can help determine why your symptoms are continuing. There may be an underlying cause that needs to be addressed with supplemental testing, strategic medical imaging or follow-up care.

4. What Are Some Risk Factors for Angioedema?
Repeated use of certain prescription and over-the-counter drugs, including NSAIDs, aspirin, penicillin, naproxen, ibuprofen and blood pressure medications, may increase the risk of developing the condition. These drugs are usually harmless, but they can create additional risk given their ability to thin the blood, affect the heart rate, increase or decrease blood pressure and affect the immune system.
Pre-existing medical ailments that weaken the immune system, such as hepatitis, AIDS, HIV, HPV or bacterial infection, may also increase the likelihood of angioedemic outbreak in your skin. When the body is routinely fighting ongoing infection or battling an auto-immune disorder, the risk of subcutaneous swelling may increase. A person who has had a previous angioedemic episode may be at risk for future episodes.

5. When Should I Seek Medical Care?
If you or a family member begins to show signs of a swelling reaction, you should make sure to monitor symptoms carefully. Listen to what the person is saying, believe them, and write down what they are saying, along with any obviously visible symptoms. When inflammation and redness occur rapidly, it could be a sign of a severe reaction that may require immediate medical attention.
This is especially true when the face and mouth are affected, since swelling in these areas may obstruct breathing, potentially leading to loss of consciousness and cardiac arrest. If a reaction has led to difficulty breathing, call 911 and describe the situation. Trained paramedics will talk you through how to open an obstructed passageway, if necessary, and keep the person alert for as long as possible.

6. What Are My Treatment Options?
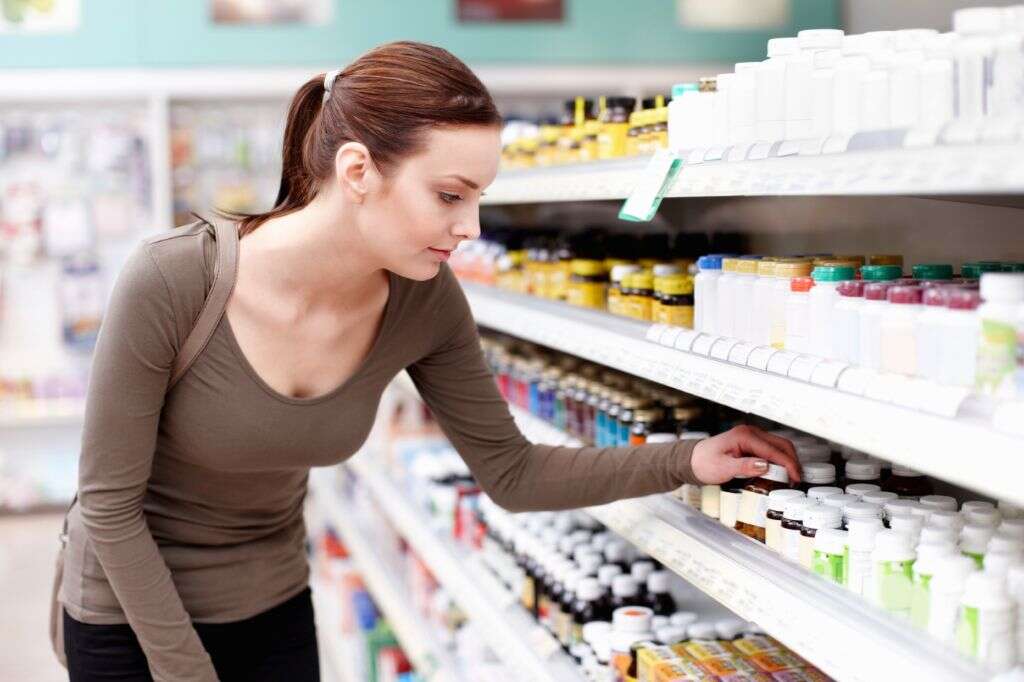
In a non-emergency situation, there are a variety of over-the-counter solutions available, including topical antihistamine creams, pills and eye drops. Other inexpensive home remedies include dampening a cool washcloth with water and applying it to the swollen area. Consider taking a cool, comfortable bath as well, so the water can soothe all parts of your body at once and regulate the nervous system.
If these DIY remedies are eventually found to be ineffective, consider seeing a doctor or allergen specialist who can prescribe a higher dosage of similar drugs, or offer other prescription-only drugs. Some anti-itch medications can be taken orally, while others require an injection. You may want to ask your doctor for an antihistamine that will reduce the effects of angioedema without making you drowsy. Another option for severe swelling and discomfort is taking a steroid, such as corticosteroids (taken orally).
7. When Was Angioedema First Discovered?
Hereditary angioedema was first scientifically cataloged by William Osler in 1888. Later, in 1963, further research was able to successfully isolate the specific genetic deficiency that causes angioedema to be inherited and passed down through the generations. This allowed for chemists, internal medicine residents, researchers, and epidemiologists to formulate coherent theories for how to treat angioedemia.
Therapeutic drugs were then developed by research and development companies, labs and universities as a way to specifically target and remedy this hereditary flaw. Closer to the 21st century, over-the-counter medications were developed to treat the symptoms of nonhereditary angioedema. Now it is possible to self-treat minor symptoms, call a pharmacist to remedy moderate symptoms, and get adequate same-day medical care from doctors and specialists.

8. What Can I Do To Proactively Prevent Angioedema?
Avoid likely triggers such as substances and environmental toxins. Regularly shower in a well-ventilated lavatory, with daily changes of clothes to ensure that pet and animal dander are not routinely re-entering your skin, bloodstream and airways. If it is not automatically easy to avoid environmental triggers or foreign substances, keep an epi-pen on hand (norepinephrine).
Wearing loose-fitting, smooth clothing made of natural fibers can also reduce inflammation and risk of outbreak. Having topical antihistamines on hand, such as tripelennamine or diphenhydramine, can help soothe rashes and discomfort. Avoid direct sunlight if you have had a recent episode, as the intensity of UV rays may aggravate the swelling.

9. How Is Angioedema Different In Adults vs Children?
It is often scary to see one’s own child showing signs of angioedema. A child experiencing swelling, redness, itching and pain—possibly for the first time—will need a different set of treatment options than an educated adult who has experienced similar discomforts before. If your child is experiencing obvious discomfort, stay calm, and observe their symptoms. Additionally, drugs and treatments that are meant for adults may actually be harmful to children.
The causes of angioedema in children can be different from adults. While adults may have built up years of resistance and immunity to certain environmental triggers, a child may encounter an allergen for the first time and have a more serious reaction. Remember that the first step to helping the child, is believing what they say, then looking for objective confirmation. Finally, never give a child a prescription drug that is intended for adults.

10. What Is the Latest Research About Angioedema?
Recent research suggests that what appears as simple swelling of the subcutaneous tissue may actually be a more serious problem called mastocytosis. Mastocytosis occurs when mast cells build up underneath the skin, and cause pain or swelling similar to angioedema. Scientists and physicians are currently researching instances of both conditions in order to determine the differences early on, and develop appropriate solutions for each.
Research is also being conducted on the effectiveness of certain immunomodulators. Unlike immunosuppressants that suppress immune system responses rapidly, immunomodulators may be able to control the intensity of immune response to antibodies incrementally, allowing for more targeted and less risky treatment options. Yet other studies are being done on the relationship between patients with asthma and patients with recurring angioedema since the two conditions present similar symptoms.