What Is Acute Otitis Media?
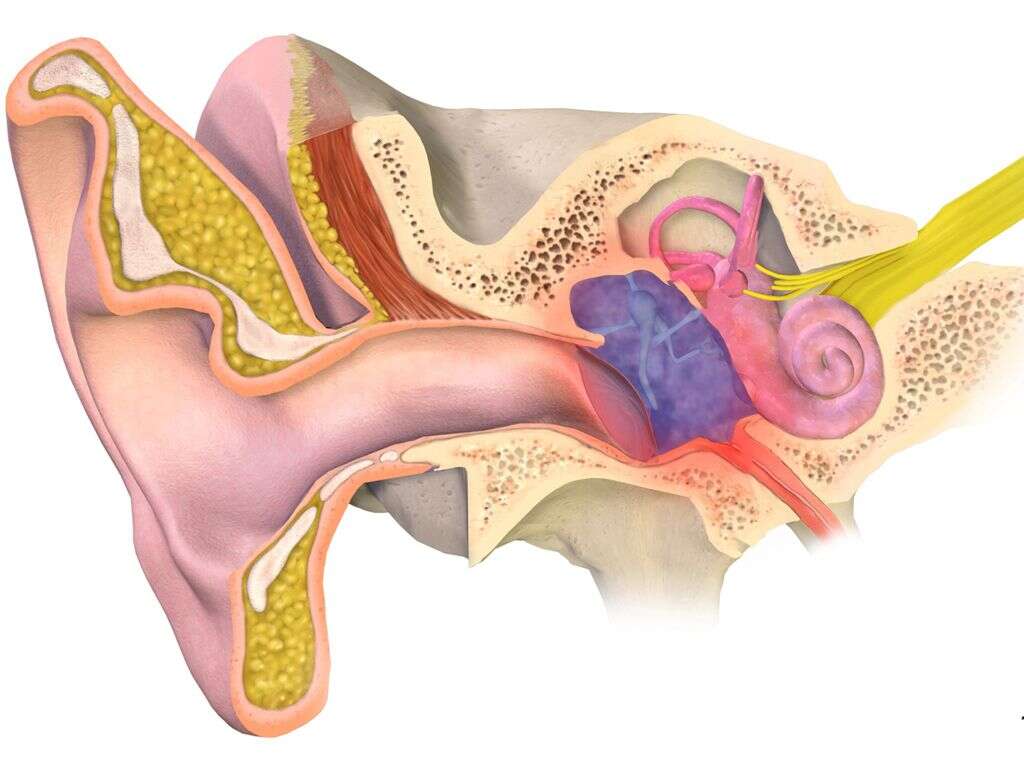
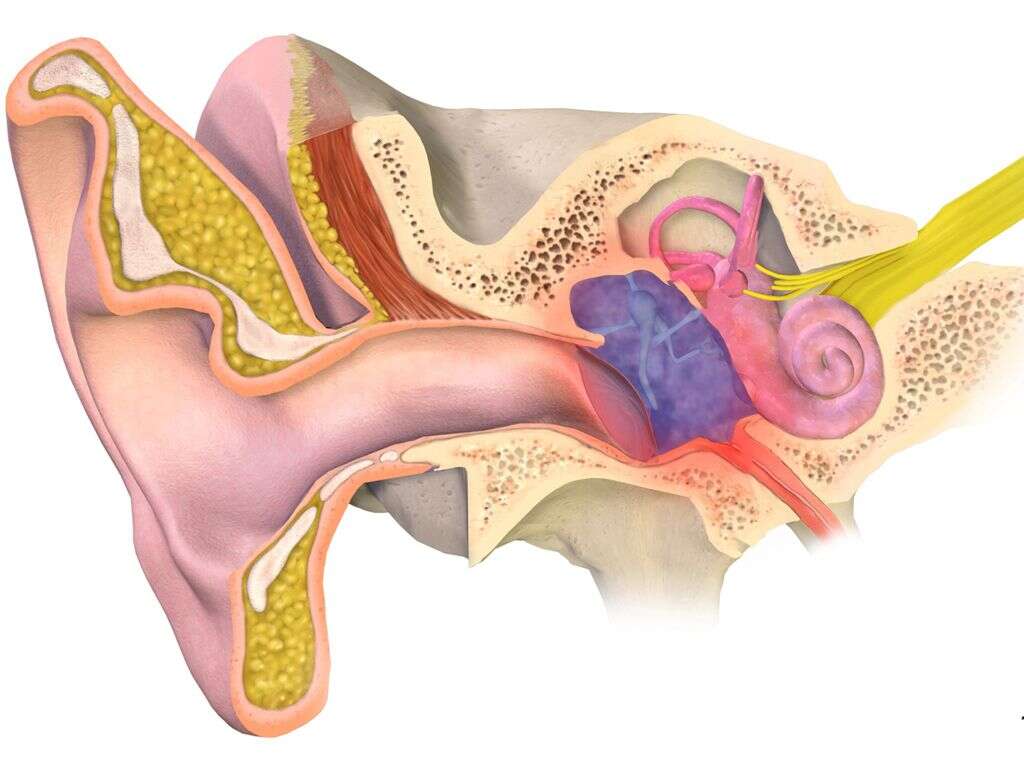
The human ear consists of three distinct sections. The middle ear is located in between the eardrum and the round window of the inner ear. One of its features is the Eustachian tube. It connects the middle ear to the back of the throat, also called the pharynx, and exists to prevent pressure from building up in the ear by opening up whenever you swallow. Acute otitis media is a painful inflammation of the middle ear due in part to a blockage of the Eustachian tube.
While both adults and children can develop AOM, it is much more common in children, particularly infants and toddlers. There are several reasons for this, but one of the most significant is that children’s Eustachian tubes are still developing. When children are very young, the Eustachian tubes are shorter, more horizontal and narrower. Therefore, they do not drain as effectively as those of adults and are more likely to become clogged.
1. Causes
Acute otitis media usually starts with congestion and swelling of the throat, nasal passages, and Eustachian tubes. This may occur due to a viral upper respiratory infection, such as influenza or the common cold. Allergies may also lead to an ear infection by causing nasal congestion or by causing the adenoids to swell, blocking off the Eustachian tubes in the process.
When the Eustachian tubes are clogged or blocked off, fluid in the ear cannot drain effectively from them. The buildup of fluid can provide an ideal environment for bacteria to grow, and the middle ear becomes infected as a result. The species of bacteria most often responsible for acute otitis media include Haemophilus influenzae, Moraxella catarrhalis, and Streptococcus pneumoniae. However, AOM isn’t always the result of a bacterial infection.
2. Prevalence
Middle ear infection is most prevalent among the young. Adults ages 25 to 85 accounted for only 1.5% to 2.3% of all acute otitis media cases in a 2005 study, while those aged 15 to 24 years made up 3.1% to 3.5%. Approximately one-half to one-third of all middle ear infections occurred in children younger than 5, while children aged 5 to 14 accounted for 19% to 22% of all cases.
As of 2016, about 50% of all children experience acute otitis media before the age of 1. However, this represents a decrease compared to recent decades. AOM incidence rates have seen an overall decrease in all age groups. Researchers theorize this may be due to increased breastfeeding of infants and routine vaccination against respiratory disorders in both children and adults.
3. Symptoms
If you are an adult with acute otitis media, you may experience ear pain that can range from mild to severe and usually occurs only on one side. Due to the presence of fluid in the middle ear, your hearing may become muffled. You may experience drainage of pus from the ear if, as sometimes happens, the eardrum bursts due to the buildup of fluid. This may cause relief of the pain, at least temporarily.
Children with AOM may experience the same symptoms as adults. However, a number of other symptoms may also be present, such as loss of appetite, headache, fever, trouble sleeping and loss of balance. If your child is too young to describe his or her symptoms to you, pay attention to signs such as increased fussiness, crying, or irritability and excessive pulling or tugging at the ear. Some children also experience symptoms of diarrhea or vomiting.
4. Diagnosis
In addition to your verbal description of the symptoms, a doctor also bases a diagnosis of acute otitis media on the appearance of the eardrum. An otoscope is a lighted instrument that the doctor uses to look inside the ears during a physical examination. A healthy eardrum appears clear when examined with the otoscope. If infection is present, the eardrum will typically appear cloudy and opaque due to the buildup of fluid behind it. The fluid buildup also causes the eardrum to bulge visibly. It may be red due to irritation.
An otoscope examination is typically sufficient to diagnose acute otitis media. However, if a closer look at the membrane of the eardrum is required, your doctor may refer you to an ear, nose, and throat specialist for a test called otomicroscopy. A doctor may also wish to measure the eardrum’s movement with a test called tympanometry.

5. Treatment
When acute otitis media is caused by bacteria, your doctor may prescribe antibiotic medication. However, it is important to determine whether the cause is bacterial and if the infection is likely to resolve on its own to avoid prescribing antibiotics unnecessarily. Otherwise, strains of bacteria can develop an immunity to the medication and be harder to treat in the future. When antibiotics are appropriate, doctors typically prescribe amoxicillin first to both children and adults with AOM. However, a different antibiotic may be prescribed to people who are allergic to amoxicillin or otherwise unable to take it.
Another possible treatment for ear infection is the placement of tubes in the eardrum. This requires a surgical procedure called a myringotomy to cut a tiny hole in the eardrum and place a small tube that allows the fluid to drain out. Myringotomy is an outpatient procedure reserved for children with certain medical conditions. Those who have recurrent, frequent ear infections may be candidates for ear tubes.

6. Complications
The buildup of pressure from fluid in the middle ear can cause the eardrum to rupture. This is usually not a very serious complication as the damaged membrane typically heals on its own within a few days. However, sometimes the damage to the eardrum does not heal. When this occurs, it may be necessary to repair the membrane surgically. Sometimes the damage may be permanent, in which case significant hearing loss can result.
AOM that does not receive adequate treatment can spread to nearby tissues. A serious infection of the middle ear may even spread to the brain, although this is rare. More common is mastoiditis, an infection of the bony protrusion behind the ear. Mastoiditis can cause damage to the bone.
7. Risk Factors
Adults and children who have an obstruction of the Eustachian tube are at greater risk for acute otitis media. Examples of obstructions include scar tissue and malignant growths. Sometimes there is negative pressure of the middle ear due to Eustachian tube dysfunction. This can also lead to AOM in patients of all ages if the dysfunction persists into adulthood. Other significant risk factors for ear infections, in children as well as adults, include frequent upper respiratory infections and allergic congestion.
Young children who are bottle-fed are at greater risk for ear infection compared to those who are breastfed. There are two reasons for this. First, feeding a baby from a bottle may allow the formula to flow backwards into the baby’s Eustachian tubes. Second, breast milk contains antibodies from the mother that help to protect against infections. Children are also at greater risk for AOM if they live in a household where adults smoke or if they spend a lot of time around other children, such as siblings or other kids at daycare.

8. Recovery
Even without antibiotics, mild cases of acute otitis media may resolve themselves within a matter of days. This occurs in the majority of cases. When antibiotics are indicated, they are usually prescribed for five to seven days. It is important to finish a prescription of antibiotics even when you or your child starts to feel better to prevent the bacteria from becoming resistant to them.
It is often necessary to manage the pain from AOM while waiting for the infection to clear up on its own. If there is no rupture of the eardrum, your doctor may give you ear drops that contain an anesthetic medication to numb the pain. Your doctor may also recommend an over-the-counter pain reliever, such as ibuprofen or acetaminophen. Follow instructions for administering these medications to children and avoid giving a child aspirin.

9. Prognosis
Most children and adults recover from acute otitis media with no long-term adverse effects. However, an infection that spreads to the brain can cause serious and sometimes permanent damage. An untreated ear infection can also cause meningitis, which is inflammation of the membranes that surround the brain. This, too, can result in death or permanent complications.
Some children may be prone to recurrent ear infections, especially if multiple risk factors are present. Due to the short-term effect that AOM can have on the hearing, children who have frequent ear infections may experience speech delays.

10. Prevention
One of the most effective preventative measures against acute otitis media is preventing the upper respiratory infections that often give rise to them. Talk to your doctor about vaccinations against influenza, pneumonia, and bacterial infections. Practice good hygiene as it relates to handwashing and covering coughs and sneezes, and teach it to your children as well. Do not smoke and keep yourself and your children away from second-hand smoke.
If you have a new baby, doctors recommend breastfeeding your baby for at least the first six months of life. This offers other health benefits beside the prevention of ear infections. However, if you choose to or must bottle-feed, be sure to hold the baby in an upright position. Do not leave the bottle in the baby’s crib.












