What Is Uveitis?
You are probably familiar with the cornea, retina, pupil and lens of the eye. These specific structures are located within three main layers that make up the eyeball. The middle layer is called the uvea, is loaded with blood vessels and supplies blood to the retina. Uveitis is swelling of the middle layer of the eyeball.
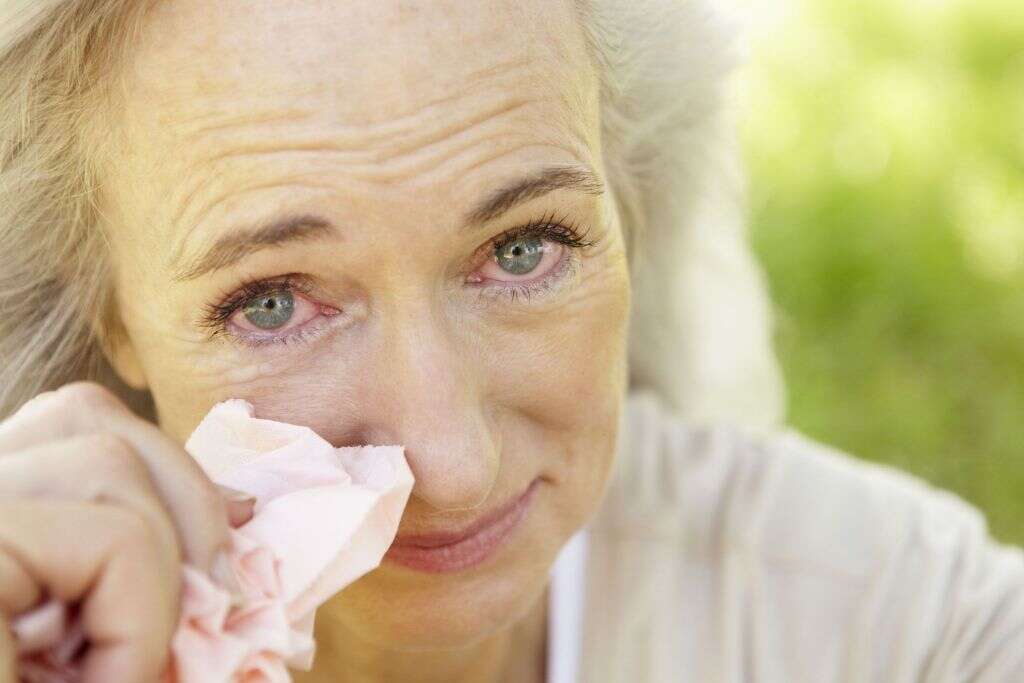
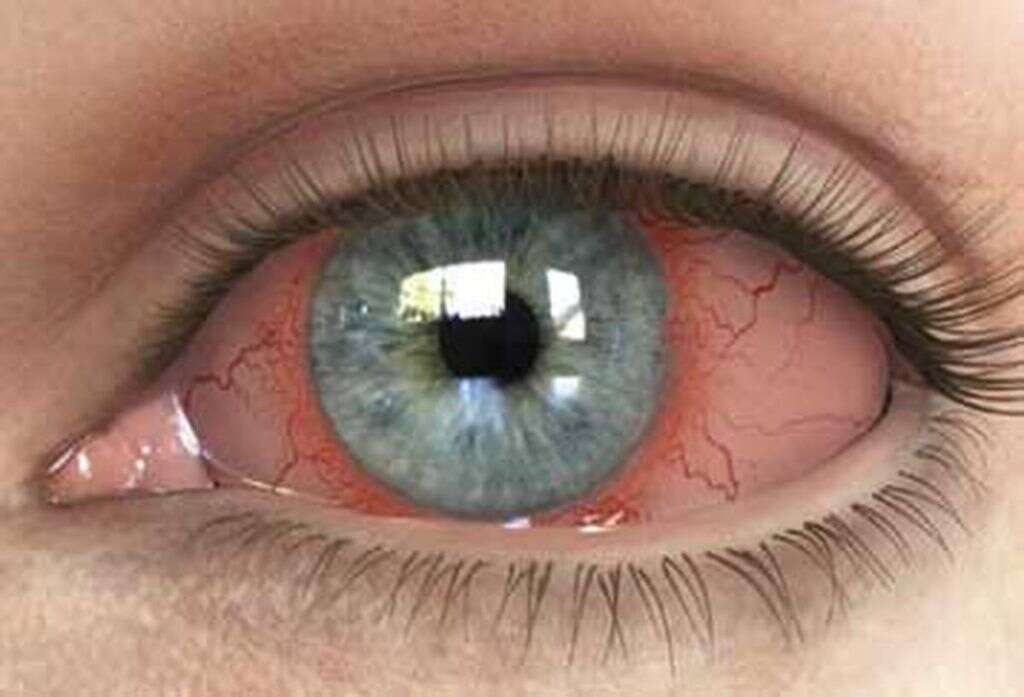
Uveitis is generally accompanied by redness and irritation. For many people, it is also incredibly painful. Proper treatment and care can help alleviate symptoms and address the potential causes of the condition. If left untreated, uveitis can lead to permanent damage to the sensitive tissue of the eyeball. Here are 10 things you should know about this painful and potentially dangerous eye condition.

1. What Is Uveitis?
Inflammation that affects the uvea is known as uveitis. It can occur suddenly, and many people experience recurring episodes of inflammation. Early diagnosis can help alleviate symptoms quicker and address any underlying causes of irritation.
Uveitis may affect one or both of the eyes. It can happen to anyone at any age. Individuals who have autoimmune disorders or certain genetic mutations may be more likely than others to experience inflammation of the uvea. Additionally, smoking increases your chance of developing uveitis.

2. What Are the Common Symptoms?
Uveitis is an inflammatory condition. As such, inflammation is the most common symptom of it. Most people will also experience redness and irritation. Pain is not uncommon, especially if the condition is not treated promptly.
You may experience dark spots within your vision, known as floaters, due to inflammation. Light sensitivity is also very common. Some people do not experience any symptoms and only find out about the condition at a routine eye exam.

3. What Are the Three Types of Uveitis?
Uveitis can affect one or more portions of the uvea. It is diagnosed and classified into three main types based on which parts are primarily displaying symptoms. The most common form is known as anterior uveitis. It affects the iris in one or both eyes. It is generally diagnosed in otherwise healthy people and is relatively easy to treat.
Intermediate uveitis occurs within the central portion of the uvea. It has an increased link to certain autoimmune disorders like multiple sclerosis. Posterior uveitis occurs when there is swelling of the choroid in the back of the eye. It is often caused by a bacterial, fungal or parasitic infection, but may also be caused by an autoimmune disease. It can lead to serious and permanent damage to the eye if left untreated.
4. Does Uveitis Affect Vision?
Floaters and blurry vision are the most common vision problems associated with uveitis. However, they aren’t the only ones. In some cases, particularly those involving chronic inflammation, the retina itself can become inflamed. This is known as retinal edema.
Some of the more serious complications that can result include glaucoma, cataracts, damage to the optic nerve, and retinal scarring or detachment. Any of these conditions can cause permanent impairment or total loss of vision.

5. What Causes Uveitis?
There are several factors that can contribute to uveitis. When it occurs in otherwise healthy individuals, the cause is often never determined. It can be the result of exposure to a toxin or trauma from an injury or surgery.
Autoimmune disorders that produce inflammation, such as rheumatoid arthritis and Crohn’s disease, are common causes of uveitis. Some cases are the result of an infection. This can be bacterial, fungal or viral. Herpes, HIV, toxoplasmosis, and West Nile virus are all frequently responsible for a uveitis diagnosis.

6. Can It Be Prevented?
Proper eye care and good hygiene practices can reduce your likelihood of contracting an infection that leads to uveitis. Avoid touching or rubbing your eyes, especially if you haven’t just washed your hands. If you do contract an infection of your eye, take all medication to ensure it is fully resolved. Avoid smoking since it increases your chance of developing uveitis.
For cases that are caused by an autoimmune condition, it is critical that you address the underlying cause. Always follow the advice and care instructions of your healthcare providers to avoid flare-ups.

7. How Is Uveitis Diagnosed?
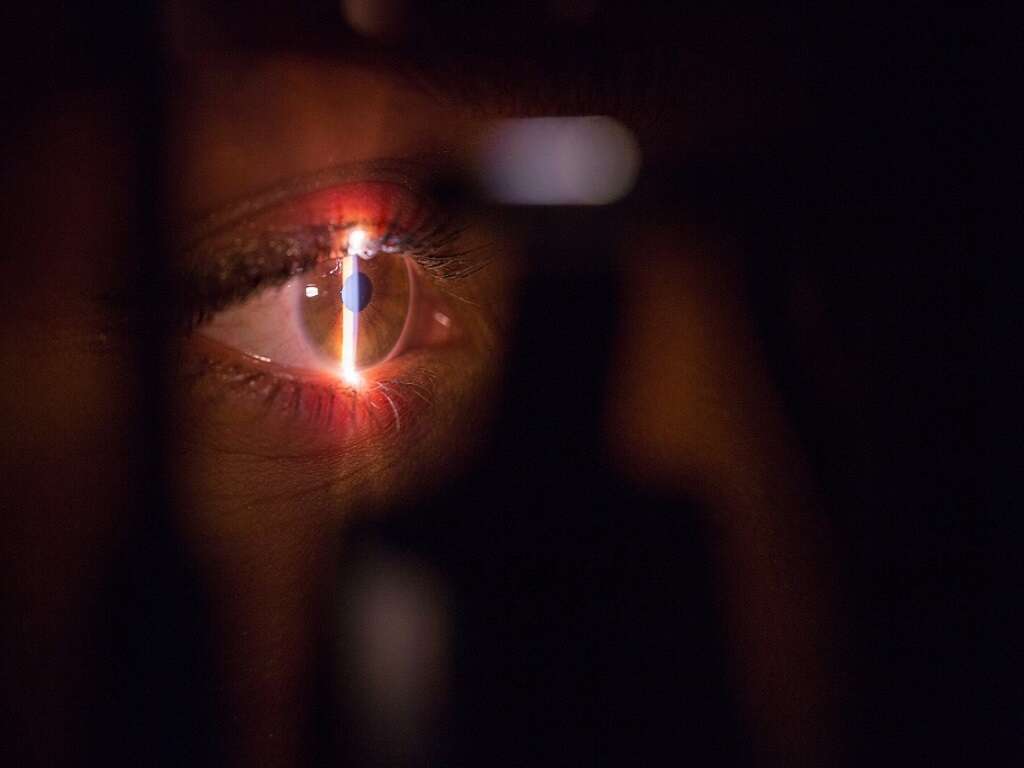
Uveitis can often be diagnosed with a physical exam of the eye. A full health history will likely be needed to help identify any conditions that may increase your likelihood of developing it.
Your doctor may perform several tests to rule out other possibilities and establish the cause of your inflammation. These can include blood work, x-rays or other imaging tests, an examination of the eye fluid and skin tests. Combined, these can give a good picture of not only the inflammation but also what is causing it. This allows for more effective and targeted treatment of the symptoms and the underlying causes of them.

8. What Type of Doctor Treats Uveitis?
Your primary care doctor may be able to provide a diagnosis of uveitis. However, as with any disease or condition of the eye, it is best to seek care from an ophthalmologist for uveitis.
Ophthalmologists are medical doctors that have received additional specialized training in the structure of the eye and conditions that affect it. They have the knowledge and equipment to make a definitive diagnosis. Additionally, they have likely seen many other cases of uveitis and can provide treatment that will effectively relieve symptoms and clear up underlying causes.

9. What Treatments Are Available?
There are several treatment options that can be used to address symptoms of uveitis. Drops are often prescribed to relieve redness and irritation. Over the counter pain medications and anti-inflammatories can also help make you more comfortable. Dark glasses can help relieve light sensitivity.
Many patients diagnosed with uveitis will be given steroids to help counter the inflammation. Drops are commonly used, although oral steroids may also be given in more severe cases. In cases of bacterial uveitis, and antibiotics can be administered orally or directly to the affected area. In severe cases of the disease, drugs may be used to suppress the immune system.
10. What Is the Recovery Period Like?
The recovery process varies depending on the type of uveitis you have. Despite all of them being related, treatment and recovery can vary between the three main types of uveitis. With all cases, recurring episodes are common once an initial diagnosis has been made, especially in cases where there is an underlying autoimmune condition contributing to the inflammation.
Symptoms of the relatively common anterior uveitis usually subside within a few days of starting treatment.
Intermediate uveitis may last for weeks before you notice an improvement. Posterior uveitis is more difficult to treat and has a longer recovery period. Many people experience periods of inflammation that can last for months or longer. Permanent damage to eye tissue is possible with posterior uveitis.