What Causes Blood Clots?
Our blood is liquid in nature. When a portion of it changes from liquid to a semisolid or gel-like state, it is called a blood clot. Blood clotting is a natural process occurring when you are injured or cut to stop bleeding. Problems occur when blood clots form inside the veins. Although most of them dissolve naturally, sometimes, they do not. When a blood clot persists inside a vein, it can lead to life-threatening conditions such as pulmonary embolism.
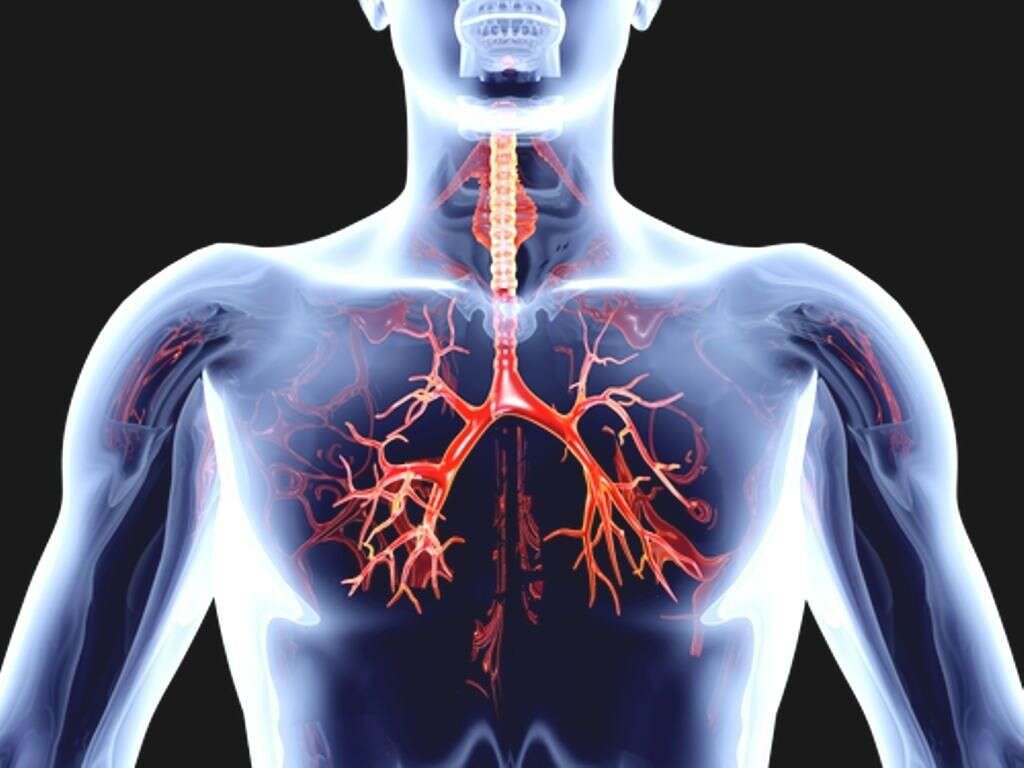
Blood clots can be either immobile or mobile. In general, immobile blood clots are not harmful. However, clots can be very dangerous when they move freely inside the circulatory system. They travel along veins to organs and may cause blockage in blood supply. Should they reach the heart or lungs, they cause life-threatening conditions. If you think that you have a blood clot, call your doctor immediately. Your doctor will be able to dissolve the clot if there is any and diagnose the case according to your symptoms and medical history.

1. Symptoms of Blood Clots
There are two main types of blood clots: deep vein thrombosis and pulmonary embolism. Deep vein thrombosis (DVT) happens when blood clots are formed inside a deep vein. The most common site is the legs and, to a less extent, the arms. The symptoms of DVT include swelling, pain, tenderness, redness, and hotness of the affected area. The symptoms are similar to those of pulling a muscle. Pulmonary embolism means that the clot gets to the lungs. Pulmonary embolism is a life-threatening condition. The signs and symptoms include sudden dyspnea, sharp, stabbing chest pain, increased heart rate, and a bloody cough.

2. Causes of Blood Clots
Clotting is a process. It starts when flowing blood reacts with certain substances either within skin tissue or inside the blood vessels. This reaction means that there is a problem with the skin or blood vessels. The insides of the arteries usually contain cholesterol plaques.
These plaques are intact. However, if they break off, the clotting process starts. Most cases of angina and brain strokes happen due to the breakdown of these plaques of cholesterol.
3. Blood Pooling
Blood clots also develop as a result of poor flow of blood within the blood vessels. For instance, an injury inside a blood vessel can lead to blood pooling whereby blood flow slows down. As a result, platelets stick together and form blood clots that move slowly and cause problems such as a DVT.
Atrial fibrillation is a condition where one of the chambers in the heart does not beat correctly causing pooling of blood and blood clots within the heart. Atrial fibrillation that is not treated may result in a stroke.
4. Blood Clots and Chronic Diseases
Some chronic diseases increase the risk of developing blood clots inside the blood vessels. Cancers are among the most common causes of blood clots. Patients with cancer are usually older and less active physically. This is why they have a higher risk of blood clots. Inflammatory bowel diseases, such as Crohn’s disease and ulcerative colitis, also pose a risk for the formation of blood clots.
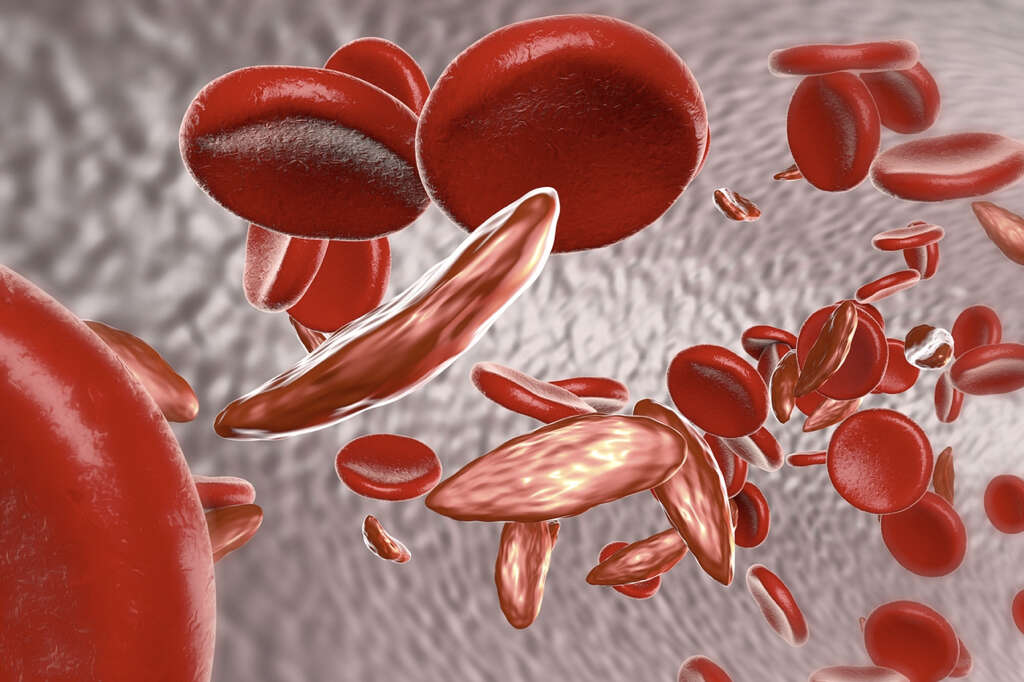
The most common theory is that inflammation causes injuries in blood vessels. Inherited clotting disorders such as sickle cell anemia cause thickening of the blood, which increases the risk of developing blood clots. Infections and autoimmune diseases also increase the risk of forming blood clots. However, the exact mechanism is not clear.
5. Complications
Complications of blood clots differ according to the affected areas. Clots in a leg or an arm can cause DVT. Clots are dangerous because they cut off blood supply to the limb and may move up to the heart, lungs, or brain. If a blood clot reaches the heart, it can cause a heart attack. Severe abdominal pain and food poisoning-like symptoms may be an indication of a blood clot in one of the abdominal blood vessels.
Blood clots are also a common cause of brain strokes. Symptoms of a blood clot in the brain include sudden headaches, the inability to speak, and sudden loss of vision in one or both eyes. If a blood clot reaches the lungs, it causes pulmonary embolism, which can be fatal if not treated immediately.

6. Disease Process
To understand the nature of harmful blood clots, we have to know how the natural clotting process happens first. In case of damage to a blood vessel, platelets accumulate and form a plug. They adhere to the injured area trying to stop the bleeding. The clot increases in size by the actions of some proteins and enzymes making it more durable.
These actions are limited in order not to exceed the injured area. Once the damaged tissues heal, the clot starts to dissolve naturally. Harmful blood clots arise when they do not dissolve and persist inside a blood vessel. Problems begin when the blood clot prevents blood from reaching tissues.

7. Diet and Lifestyle Changes to Ease Blood Clots
If you suffer from frequent clotting, you need to make some diet and lifestyle adjustments to improve the condition. Be sure to talk to your healthcare provider on the best ways to make the correct life style changes for you. Some healthy changes may actually interfere with blood thinning medications or put you at risk for dislodging clots.
You could ask you provider about some of these common diet and exercise changes that some have found helpful: For starters, drink more water because dehydration is one of the common causes of having thick blood. Some sources suggest red wine (in moderation), grape juices, kiwis, and virgin olive oil to decrease the risk of blood clots. In addition to these foods, garlic, cinnamon, turmeric, and cayenne peppers may be considered natural blood-thinners. Also, cut out animal fats because they are bad for your cardiovascular system; however, some nutrition experts debate this fact. You also need to exercise on a regular basis. Physical activity is one of the best ways to improve your general health, especially the health of your cardiovascular system.

8. Diagnosis
The diagnosis of blood clots is usually made from the symptoms of the patient. The physical examination will show swelling, discoloration, hotness, and tenderness of the skin. In addition to clinical evaluation and physical examination, your doctor may suggest performing some tests. Ultrasounds show clots. They are usually visible in the image.
A series of images may be useful to determine whether the clot is growing or not. D-Dimer is a substance found in large amounts in the blood of people who develop clots frequently. Venography, CT, and MRI can show whether you have blood clots or not. Venography may be replaced with ultrasound since the latter is less invasive.

9. Treatment
The treatment aims at preventing blood clots from moving around or getting bigger. Blood thinners, or anticoagulants, decrease the ability of blood to form clots. Blood thinners can be administered intravenously, intradermally, or orally.
Medications include heparin, enoxaparin, dalteparin, fondaparinux, warfarin, dabigatran, rivaroxaban, apixaban, and edoxaban. Aspirin is another more conservative blood thinner available. A physician is trained to choose the best combination of treatment for the individual. In life threatening emergent situations, a physician may order a clot buster or thrombolytic drug. Filters inserted in large veins are the best option for patients who cannot take medications. The most commonplace of filters is the inferior vena cava. It prevents blood clots from reaching the heart or lungs.

10. Long-Term Outlook
Blood clots are serious. They reduce or cut off blood supply to tissues, which may lead to serious health problems. Once you feel the symptoms of having a blood clot, you should see your doctor immediately. In addition, taking your medications, following a healthy diet, and exercising regularly decrease the risk of having blood clots.
You can lead a perfect life even if you have had a blood clot. Still, you may need regular follow-up if you have frequent blood clots. In general, the condition is treatable and patients lead fairly normal lives.