Hyperventilation Definition, Causes & More
 Article Sources
Article Sources
- 1. 'Hyperventilation.' Michigan Medicine, University of Michigan, www.uofmhealth.org/health-library/hypvn.
- 2. 'How Correct Breathing Reduces Anxiety.' No Panic, 6 Mar. 2020, nopanic.org.uk/important-breathe-properly-help-anxiety.
- 3. 'Causes of Hyperventilation.' Alberta.ca, myhealth.alberta.ca/health/Pages/conditions.aspx?hwid=aa141603.
- 4. Robson, Andrew. 'Dyspnoea, Hyperventilation and Functional Cough: a Guide to Which Tests Help Sort Them out.' PubMed Central, www.ncbi.nlm.nih.gov/pmc/articles/PMC5343732.
- 5. Tilles, Ira H. 'Hyperventilation Syndrome Symptoms, Causes, Effects & Treatment.' EMedicineHealth, www.emedicinehealth.com/hyperventilation/article/em.htm.
- 6. 'Diabetic Ketoacidosis.' Nhs.uk, www.nhs.uk/conditions/diabetic-ketoacidosis.
- 7. Bogossian, Elisa G., et al. 'Hyperventilation in Adult TBI Patients: How to Approach It?' Frontiers, www.frontiersin.org/articles/10.3389/fneur.2020.580859/full.
- 8. Pantelyat, Alexander, et al. 'Central Neurogenic Hyperventilation: A Sign of CNS Lymphoma.' PubMed Central, www.ncbi.nlm.nih.gov/pmc/articles/PMC5759985.
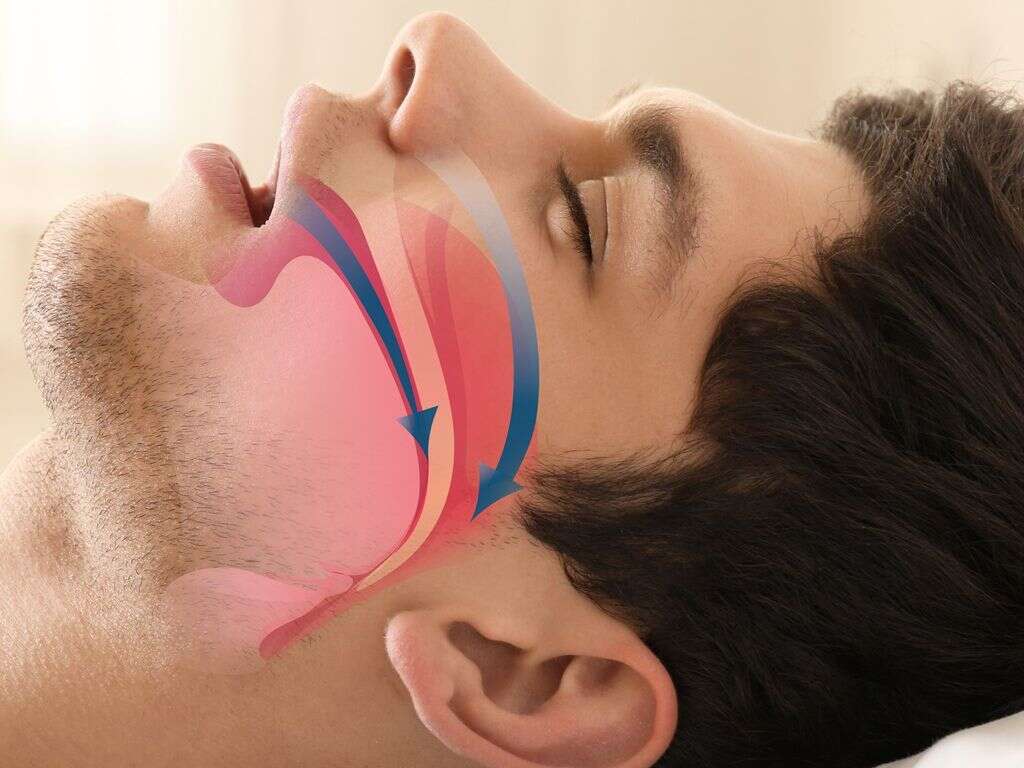
When you inhale, air enters in the lungs and oxygen from air moves from lungs to blood. At the same time, carbon dioxide moves from blood to lungs and is exhaled. This gas exchange is essential to life.
Hyperventilation is a sudden onset of heavy breathing where the body expels more carbon dioxide than normal. If prolonged, hyperventilation can manifest in other parts of the body, as the blood flow is imbalanced between carbon dioxide and oxygen. Symptoms to look for include lightheadedness, nausea and a tingling sensation in the fingertips. Forced regular breathing can return the balance and restore blood oxygen and carbon monoxide levels.

1. Is Hyperventilation Dangerous?
Hyperventilating in itself isn't dangerous or life-threatening; however, it may lead to situations that can cause serious harm. Fainting and lightheadedness can both cause serious injuries.1‘Hyperventilation.’ Michigan Medicine, University of Michigan, www.uofmhealth.org/health-library/hypvn. If the event is triggered by anxiety or stress, it could lead to other problems down the line unless it's monitored by a healthcare professional.
It may also be an indication that something else in the body isn't working optimally. For example, hyperventilation can indicate that the body is unable to balance oxygen and carbon dioxide levels in the blood, which may indicate cardiovascular or pulmonary conditions.

2. Understanding Hyperventilation Syndrome
Hyperventilation is not a common occurrence for many, and when it happens it tends to be a once-off. When the frequency of events increases, a patient may be diagnosed with hyperventilation syndrome. It can have many of the same causes as regular hyperventilation.
Hyperventilation syndrome can increase anxiety and stress. Stress management and breathing exercises are recommended to curb the effects of hyperventilation syndrome until the cause of the irregular breathing is diagnosed.

3. Anxiety & Stress
Anxiety is one of the major causes of hyperventilation. Research reveals that around 60 percent of panic attacks are accompanied by hyperventilation. During a panic attack, the body releases a stress hormone called adrenaline. This immediately picks up the heart rate as the body goes into fight-or-flight mode.
Controlled breathing, which is practiced by using a paper bag, is one of the measures to regulate breathing. It's important for the body to relax before relaxed measured breathing can take place again.2‘How Correct Breathing Reduces Anxiety.’ No Panic, 6 Mar. 2020, nopanic.org.uk/important-breathe-properly-help-anxiety.

4. Use of Stimulants or Drugs
Breathing is not always a natural response, and for some, ingesting stimulants, such as caffeine, and drug overdoses of substances like aspirin, amphetamines and cocaine, can alter breathing. Even asthma medication and ingesting too much iron can cause irregular breathing.3‘Causes of Hyperventilation.’ Alberta.ca, myhealth.alberta.ca/health/Pages/conditions.aspx?hwid=aa141603.
The result is hyperventilation, and known treatments include physician intervention, especially in the event of an overdose. A strict rehabilitation program might be needed if simple lifestyle changes aren't effective. Continuous hyperventilation may result in stress.

5. Bleeding or Severe Pain
Excessive bleeding can reduce blood oxygen levels, which means the cardiovascular system has to work overtime to get enough red blood cells to organs. When the blood is starved of oxygen, these organs can't work properly, including the lungs. A lack of oxygen can cause hyperventilation.
Severe pain may also trigger adrenaline, which is known to activate stress hormones in the body and results in hyperventilation. Short, shallow breaths don't produce the balanced oxygen to carbon dioxide ratios that deep breaths do.

6. Respiratory Diseases
When hyperventilation syndrome is diagnosed, patients go through a series of tests to rule out respiratory disease as the underlying condition. Chronic Obstructive Pulmonary Disease, or COPD, and asthma are two of the most common respiratory causes of hyperventilation.
COPD is a chronic condition where lung function deteriorates over time, and the reduced lung capacity can cause delays in the response to breathing triggers. Pulmonary fibrosis occurs when lung tissue is scarred or damaged and may also cause hyperventilation.4Robson, Andrew. ‘Dyspnoea, Hyperventilation and Functional Cough: a Guide to Which Tests Help Sort Them out.’ PubMed Central, www.ncbi.nlm.nih.gov/pmc/articles/PMC5343732.

7. Cardiovascular Diseases
Hyperventilation can be an indication that a person may have a heart condition. Rapid breathing, panic and a feeling of impending doom are symptoms of panic attacks and heart conditions, such as a heart attack, also referred to as a myocardial infarction.5Tilles, Ira H. ‘Hyperventilation Syndrome Symptoms, Causes, Effects & Treatment.’ EMedicineHealth, www.emedicinehealth.com/hyperventilation/article/em.htm.
These conditions also result in chest pains and a tingling sensation in the fingers. People who experience these issues should err on the side of caution and go to the emergency room to rule out a heart attack.

8. Diabetic Ketoacidosis
One sign of diabetic ketoacidosis, or DKA, is rapid breathing, which can result in hyperventilation. This condition also has crossover symptoms with hyperventilation, such as sleepiness, dizziness, disorientation and fainting.6‘Diabetic Ketoacidosis.’ Nhs.uk, www.nhs.uk/conditions/diabetic-ketoacidosis. DKA is a complication of high blood sugar levels, associated more often with Type 1 diabetes.
While breathing may help the person remain conscious, diabetes treatments should be administered quickly. Pregnant women and those with underlying conditions should seek medical assistance immediately if DKA results in hyperventilation.

9. Head Trauma
Serious brain injuries may not cause hyperventilation. However, hyperventilation is used in the treatment of these injuries because it has a positive effect on intracranial hypertension. This is because hyperventilation causes hypocapnia, which reduces the blood flow and blood pressure to the affected area in the brain.
This extreme form of therapy is only performed under strict monitoring, as it can sometimes result in other damage to brain tissue.7Bogossian, Elisa G., et al. ‘Hyperventilation in Adult TBI Patients: How to Approach It?’ Frontiers, www.frontiersin.org/articles/10.3389/fneur.2020.580859/full.

10. Neurological Problems
Neurological conditions, such as strokes, encephalitis and meningitis, may cause breathing problems. Neurological conditions may cause a temporary change in the breathing pattern , which results in both hyperventilation and apnoea.
Central neurogenic hyperventilation, or CNH, occurs when a person breathes too fast. In around 20 percent of the cases where patients were diagnosed with CNH, they also tested positive for central nervous system lymphoma, a rare form of non-Hodgkin lymphoma.8Pantelyat, Alexander, et al. ‘Central Neurogenic Hyperventilation: A Sign of CNS Lymphoma.’ PubMed Central, www.ncbi.nlm.nih.gov/pmc/articles/PMC5759985.