Hemoptysis Definition, Causes and More
 Article Sources
Article Sources
- 1. Jacob L. Bidwell | Robert W. Pachner. 'Hemoptysis: Diagnosis and Management.' American Family Physician, aafp.org/afp/2005/1001/p1253.html.
- 2. Radchenko, C., et al. 'A Systematic Approach to the Management of Massive Hemoptysis.' PubMed Central, ncbi.nlm.nih.gov/pmc/articles/PMC5696556.
- 3. 'Hematemesis.' Cancer Therapy Advisor, 17 2019, cancertherapyadvisor.com/home/decision-support-in-medicine/hospital-medicine/hematemesis.
- 4. 'Evaluation of Hemoptysis.' Clinical Decision Support for Health Professionals, 2 2020, bestpractice.bmj.com/topics/en-us/1039.
- 5. Gershman, E., et al. 'Management of Hemoptysis in Patients with Lung Cancer.' PubMed Central, ncbi.nlm.nih.gov/pmc/articles/PMC6712256.
- 6. 'Etiology and Management of Pediatric Hemoptysis.' JAMA Network, 1 Apr. 2001, jamanetwork.com/journals/jamaotolaryngology/fullarticle/482262.
Hemoptysis refers to coughing up or spitting up blood and comes from the Greek words haima and ptysis, which mean blood and spitting, respectively. Hemoptysis is a common respiratory health problem, and in most cases, the condition heals without medical intervention.
Massive hemoptysis is the severe form of the condition, and identifying it is imperative as it's often life-threatening without urgent treatment. Diagnosing and treating hemoptysis presents challenges that may delay the urgent response required to mitigate massive hemoptysis. Consequently, doctors may employ more than one diagnostic methodology to improve patient outcomes.

1. Causes
There are several causes for hemoptysis. The most common causes include short-term or long-term bronchitis, damaged airways, lung cancer, tuberculosis, pneumonia and chronic obstructive pulmonary disease.1Jacob L. Bidwell | Robert W. Pachner. ‘Hemoptysis: Diagnosis and Management.’ American Family Physician, aafp.org/afp/2005/1001/p1253.html. Congestive heart failure, endometriosis, use of crack cocaine, a lung abscess and autoimmune and inflammatory conditions can also cause hemoptysis.
In some cases, a person may develop hemoptysis due to a parasitic infection, non cancerous lung tumors, pulmonary embolism, pulmonary arteriovenous malformations, Hughes-Stovin syndrome, sarcoidosis, use of anticoagulants and hereditary hemorrhagic telangiectasia. Foreign objects in the airway and injuries from a car accident or gunshot wound may also cause hemoptysis.

2. Symptoms
Hemoptysis may be characterized by a sudden onset of fever and coughing up bloody or blood-stained muco-purulent sputum.1Jacob L. Bidwell | Robert W. Pachner. ‘Hemoptysis: Diagnosis and Management.’ American Family Physician, aafp.org/afp/2005/1001/p1253.html. This may be a sign of acute bronchitis or pneumonia. Hemoptysis related to malignancy or infections, such as tuberculosis, may present with weight loss, night sweats and a fever.
When bronchogenic carcinoma causes hemoptysis, a person may experience a changing cough accompanied by weight loss or anorexia. Other symptoms may include fatigue and chest pain.

3. Massive Hemoptysis
Massive hemoptysis is a severe, life-threatening form of hemoptysis that requires urgent medical attention. It involves a large amount of expectorated blood or rapid bleeding.2Radchenko, C., et al. ‘A Systematic Approach to the Management of Massive Hemoptysis.’ PubMed Central, ncbi.nlm.nih.gov/pmc/articles/PMC5696556. Unlike minor hemoptysis, which most doctors encounter frequently, massive hemoptysis is rare.
Most doctors lack the adequate preparation to manage this time-sensitive condition in a prompt, systematic fashion. The doctor must implement critical initial steps to ensure the patient has the opportunity to receive more definitive treatment.
4. Physical Examination
Evaluating a patient's medical history improves the focus and accuracy of a differential diagnosis.1Jacob L. Bidwell | Robert W. Pachner. ‘Hemoptysis: Diagnosis and Management.’ American Family Physician, aafp.org/afp/2005/1001/p1253.html. Doctors record a person's vital signs, including fever, tachypnea, tachycardia, hypoxia, weight changes and pulse oximetry.
They may note the patient's constitutional signs, such as their level of distress and cachexia. Doctors may also inspect the skin and mucous membranes and examine the lymph nodes. A cardiovascular exam may be performed, along with an inspection of the chest and lungs. Finally, the doctor may examine the patient's abdomen and extremities.

5. Diagnostic Evaluation
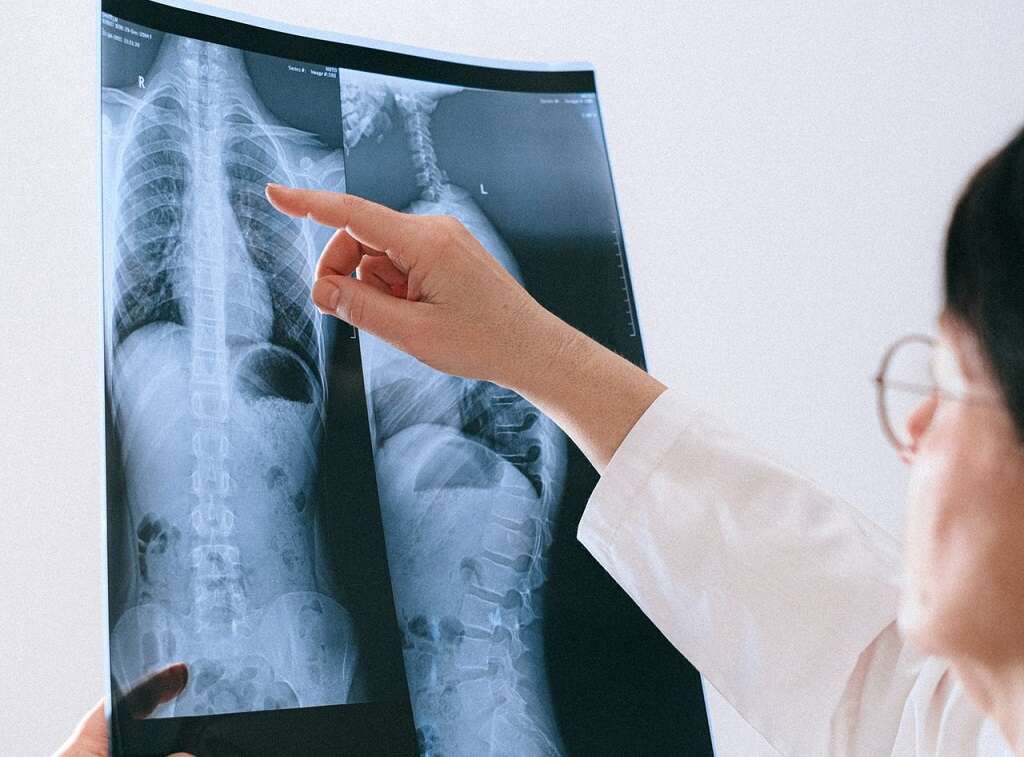
After a careful evaluation of the patient's medical history and a thorough physical examination, the doctor may obtain a chest radiograph.1Jacob L. Bidwell | Robert W. Pachner. ‘Hemoptysis: Diagnosis and Management.’ American Family Physician, aafp.org/afp/2005/1001/p1253.html. If the radiograph fails to yield a conclusive diagnosis, the doctor may request further imaging via a chest CT scan to rule out malignancy.
High-resolution CT scans are becoming an increasingly important aspect of the initial evaluation during hemoptysis diagnosis, and doctors prefer it when they suspect parenchymal disease. When hemoptysis is inexplicable or recurrent, an additional laboratory evaluation may be necessary.
6. Hemoptysis vs. Hematemesis
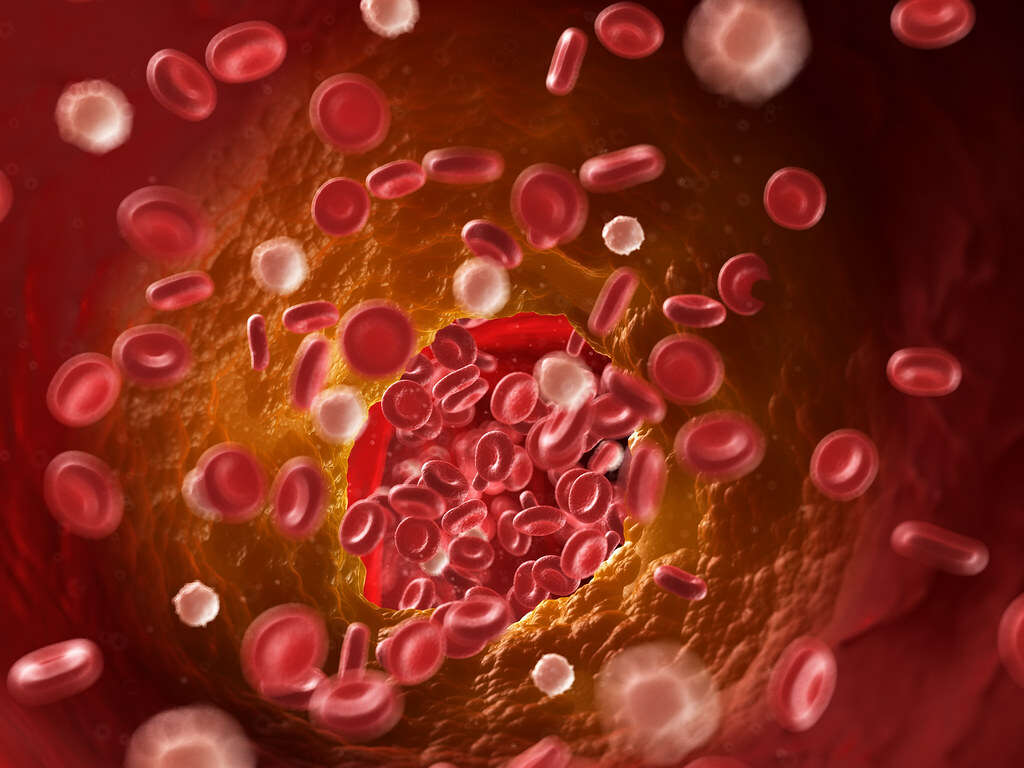
Hemoptysis can be easily mistaken for hematemesis, which is defined as vomiting up blood.3‘Hematemesis.’ Cancer Therapy Advisor, 17 2019, cancertherapyadvisor.com/home/decision-support-in-medicine/hospital-medicine/hematemesis. However, these conditions have some crucial differences. The blood in hemoptysis is bright red with a frothy consistency, while the blood in hematemesis may be either bright red or have the appearance and consistency of coffee grounds.
While hemoptysis is caused by various respiratory conditions, such as pneumonia, lung cancer, cystic fibrosis, pulmonary embolism and so on, hematemesis is caused by various gastrointestinal conditions and liver failure.
7. Hemoptysis vs. Pseudohemoptysis
Unlike hemoptysis, pseudohemoptysis involves coughing up blood from other sources, rather than from the lower respiratory tract.4‘Evaluation of Hemoptysis.’ Clinical Decision Support for Health Professionals, 2 2020, bestpractice.bmj.com/topics/en-us/1039. With pseudohemoptysis, the blood tends to be darker, and it may be caused by aspiration of hematemesis into the lungs.
It can also occur when bleeding from the mouth or upper airway triggers a cough reflex. In some cases of pseudohemoptysis, such as a Serratia marcescens infection, the expectorated material is not blood but has a similar appearance.

8. Hemoptysis and Cancer
Malignancy-related hemoptysis is common. In the U.S., it accounts for almost 25 percent of all cases.5Gershman, E., et al. ‘Management of Hemoptysis in Patients with Lung Cancer.’ PubMed Central, ncbi.nlm.nih.gov/pmc/articles/PMC6712256. Many patients with lung cancer experience hemoptysis to some extent during the course of the disease.
Even though hemoptysis related to cancer is common, managing the condition is difficult. It can present dramatically or subtly, making it a challenge for health care providers. With cancer, the rate and volume of bleeding are dependent on numerous mechanisms.

9. Hemoptysis in Children
Although hemoptysis is rare in children, it's considered potentially life-threatening when it presents as a symptom of an underlying respiratory tract infection.6‘Etiology and Management of Pediatric Hemoptysis.’ JAMA Network, 1 Apr. 2001, jamanetwork.com/journals/jamaotolaryngology/fullarticle/482262. Doctors systematically evaluate the underlying causes and implement aggressive management.
An otolaryngologist may perform a flexible endoscopy of the nose, nasopharynx and larynx as part of the diagnosis and management of hemoptysis in children. They may also perform a bronchoscopy, especially when the child experiences massive hemoptysis.

10. Management
The management of hemoptysis involves stopping the bleeding, preventing aspiration and treating the underlying cause.1Jacob L. Bidwell | Robert W. Pachner. ‘Hemoptysis: Diagnosis and Management.’ American Family Physician, aafp.org/afp/2005/1001/p1253.html. In most cases, hemoptysis is acute and mild and caused by bronchitis. Outpatient intervention via oral antibiotics and close monitoring is often enough.
Massive hemoptysis requires an urgent and aggressive approach that may involve early consultation with a pulmonologist and intensive care. If the massive hemoptysis is life-threatening, the patient may be diagnosed and receive urgent therapy simultaneously.