Dermatitis Herpetiformis Symptoms, Causes & More
 Article Sources
Article Sources
- 1. Gualandris, Federica, et al. ‘The Association of HLA-DQ2 with Celiac Disease.’ IntechOpen, IntechOpen, 31 Mar. 2021, www.intechopen.com/books/celiac-disease/the-association-of-hla-dq2-with-celiac-disease
- 2. Celiac Disease Screening.’ Celiac Disease Foundation, celiac.org/about-celiac-disease/screening-and-diagnosis/screening/
- 3. Clarindo, Marcos Vinícius, et al. ‘Dermatitis Herpetiformis: Pathophysiology, Clinical Presentation, Diagnosis and Treatment.’ Anais Brasileiros De Dermatologia, Sociedade Brasileira De Dermatologia, 2014, www.ncbi.nlm.nih.gov/pmc/articles/PMC4230654/
Dermatitis herpetiformis goes under many names, including Duhring's disease, DH, celiac rash or gluten rash. It's a chronic skin condition that causes blisters and itchy bumps. The condition's primary cause is sensitivity to gluten, a protein common in grains, such as wheat, barley and rye.
About 10 to 25 percent of people who are diagnosed with celiac disease also have dermatitis herpetiformis. Most people with this condition don't exhibit the digestive symptoms of celiac disease. Almost all dermatitis herpetiformis patients have an asymptomatic form of celiac disease. This condition is often recognized as the skin manifestation of celiac disease.

Who Is at Risk?
People of all ages can get dermatitis herpetiformis. However, people between the ages of 30 and 40 are the most likely to be impacted. People of northern European descent are at risk, and the disease affects men more commonly than it does women. Likewise, genital and oral problems occur most commonly in men.
People who have a first relative who has the skin condition are at a slightly higher risk of having it themselves. A history of autoimmune diseases in the family is also common in people with dermatitis herpetiformis. Those diseases include thyroid disease, pernicious anemia and Addison's disease.

Causes
When people with dermatitis herpetiformis eat gluten, they have an autoimmune reaction. Digestion of gluten triggers the immune system. The body produces IgA antibodies, which deposit on the skin and cause blisters and itchy, red bumps.
Genetics is an important factor in dermatitis herpetiformis. A person with a first-degree relative with celiac disease and/or dermatitis herpetiformis is five percent more likely to have the skin condition. HLA-DQ2 and HLA-DQ8 genes are closely associated with the disease.1Gualandris, Federica, et al. ‘The Association of HLA-DQ2 with Celiac Disease.’ IntechOpen, IntechOpen, 31 Mar. 2021, www.intechopen.com/books/celiac-disease/the-association-of-hla-dq2-with-celiac-disease

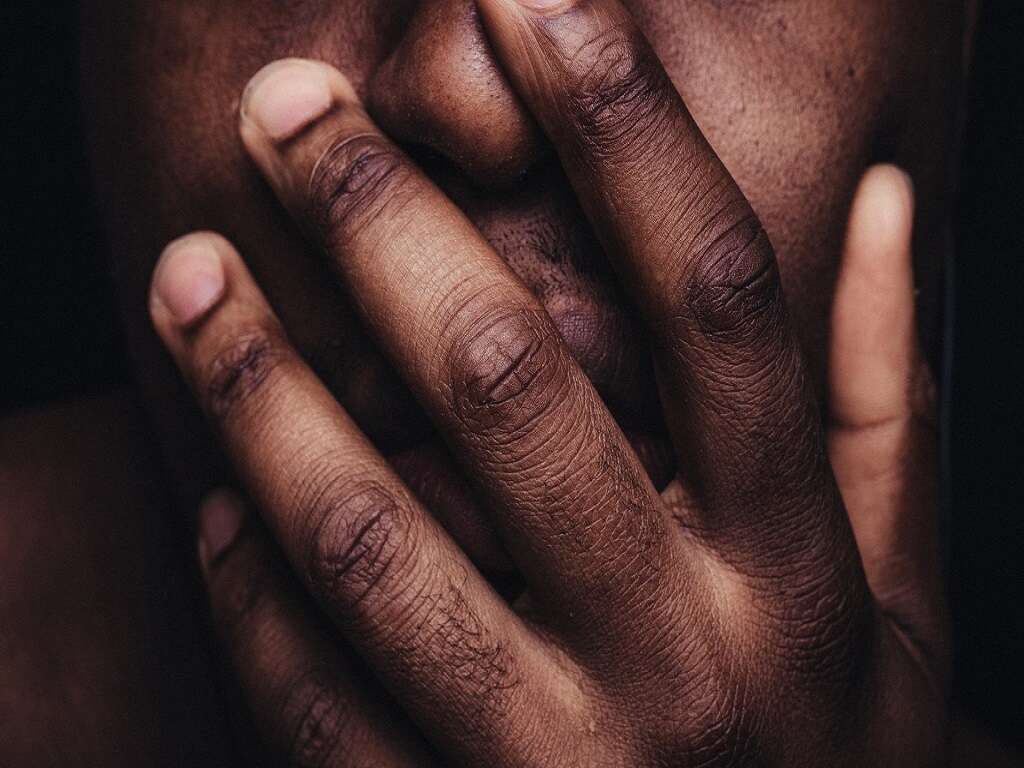
Symptoms
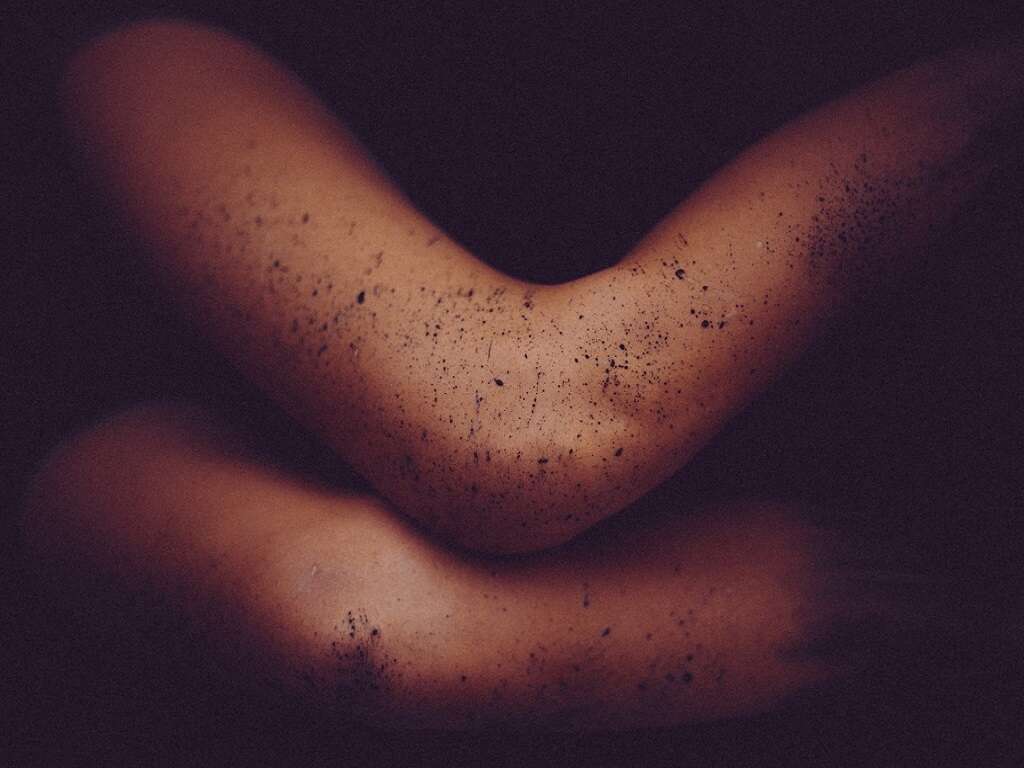
Dermatitis herpetiformis is commonly associated with skin, mouth and gastrointestinal health problems. Skin problems are a common sign of the condition. They include itchy, red bumps and blisters that may sometimes burn. These symptoms occur on the elbows, knees, scalp and buttocks.
The disease may cause tooth enamel problems that may manifest as discoloration, pitting, horizontal grooves and, in rare cases, canker sores. Gastrointestinal symptoms are rare, but when they occur, they include cramping, bloating, constipation, diarrhea and pain.

Diagnosis
A healthcare provider examines the patient's blisters and bumps. Afterward, they may perform a skin biopsy or blood test to determine whether the patient has dermatitis herpetiformis. These tests help to rule out other skin disorders.
A skin biopsy involves the extraction of a skin sample to check for evidence of the disease. A blood test checks for the presence of anti-endomysial and anti-tissue transglutaminase, two antibodies associated with celiac disease.2Celiac Disease Screening.’ Celiac Disease Foundation, celiac.org/about-celiac-disease/screening-and-diagnosis/screening/ Someone with dermatitis herpetiformis will test positive for the blood and skin tests.

Other Skin Disorders With Similar Symptoms
The differential diagnosis of dermatitis herpetiformis includes many skin disorders that cause itching and blistering. These disorders include linear IgA disease, pemphigoid, eczema and scabies, all of which are not associated with sensitivity to gluten.
Linear IgA is an autoimmune disease that certain medications may trigger. Pemphigoid is also an autoimmune disorder that presents skin, oral and genital symptoms similar to dermatitis herpetiformis. Eczema refers to skin inflammation, whereas scabies is a highly contagious skin condition caused by the Sarcoptes scabiei mite.
Complications
The same complications that occur in people who have celiac disease may also occur in those with dermatitis herpetiformis. Some of the potential complications of this skin condition include osteoporosis and certain forms of colon cancer.
People with dermatitis herpetiformis are also at risk of developing other autoimmune conditions, such as thyroid disease and type 1 diabetes. As with celiac disease, consuming a gluten-free diet reduces the risk of developing these complications.

Treatment
Dermatitis herpetiformis can be managed without drugs sometimes simply by adopting a gluten-free diet. In other cases, dapsone, an oral antibiotic, or topical steroids may be recommended.3Clarindo, Marcos Vinícius, et al. ‘Dermatitis Herpetiformis: Pathophysiology, Clinical Presentation, Diagnosis and Treatment.’ Anais Brasileiros De Dermatologia, Sociedade Brasileira De Dermatologia, 2014, www.ncbi.nlm.nih.gov/pmc/articles/PMC4230654/ If the drugs fail to provide relief, the health care provider may prescribe sulfasalazine or sulfapyridine.
A person with dermatitis herpetiformis may have to continue taking medication for one to two years to prevent further occurrence of the bumps and blisters associated with the skin condition.

Outlook
Dermatitis herpetiformis can be chronic unless a person adopts a gluten-free diet. The skin condition is not always predictable and may go away without treatment. In some cases, the site of the bumps and blisters may change color. A gluten-free diet, and sometimes medications, helps manage the symptoms of the condition.
Like other types of dermatitis, dermatitis herpetiformis is not contagious. People with this condition are at a higher risk for other autoimmune disorders, such as diabetes, pernicious anemia and thyroid disorders.

Living With Dermatitis Herpetiformis
A person with dermatitis herpetiformis can take care of themselves in several ways. They should take their medications as prescribed by their doctor. They should also ask their dietician if other dietary changes may be useful besides avoiding foods with gluten.
A gluten-free diet involves avoiding foods and ingredients such as wheat, rye, barley, beer, pastas, donuts, cookies and so on. Many processed foods contain gluten. Living with the disease and managing it successfully requires one to learn which foods contain gluten.

A Final Word
Dermatitis herpetiformis can be a difficult disease to live with. Visible bumps and blisters on the skin may make social situations awkward. The itchiness may be disruptive and may interfere with sleep.
Adopting a gluten-free diet can also be challenging because it means giving up pleasurable foods, however, there are many gluten-free foods in stores. Nonetheless, consulting a doctor to see if a gluten-free diet is right for them may be the best treatment option for some patients.