Calf Muscle Pain Causes, Treatments and More
 Article Sources
Article Sources
- 1. 'Calf Muscle.' Calf Muscle | Michigan Medicine, www.uofmhealth.org/health-library/abq4737#abq4737-sec.
- 2. 'Calf Pain.' Healthdirect, Healthdirect Australia, www.healthdirect.gov.au/calf-pain.
- 3. 'Leg Cramps at Night: Causes, Pain Relief & Prevention.' Cleveland Clinic, my.clevelandclinic.org/health/diseases/14170-leg-cramps.
- 4. 'Calf Muscle Injury.' Calf Muscle Injury | Michigan Medicine, www.uofmhealth.org/health-library/abq4844.
- 5. 'Deep Vein Thrombosis (DVT).' Mayo Clinic, Mayo Foundation for Medical Education and Research, 22 Dec. 2020, www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/symptoms-causes/syc-20352557.
- 6. 'Deep Vein Thrombosis (DVT).' Mayo Clinic, Mayo Foundation for Medical Education and Research, 22 Dec. 2020, www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/diagnosis-treatment/drc-20352563.
- 7. 'Peripheral Artery Disease (PAD).' Mayo Clinic, Mayo Foundation for Medical Education and Research, 14 Jan. 2021, www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/symptoms-causes/syc-20350557.
- 8. 'Peripheral Artery Disease (PAD).' Mayo Clinic, Mayo Foundation for Medical Education and Research, 14 Jan. 2021, www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/diagnosis-treatment/drc-20350563.
- 9. 'Sciatica: Causes, Symptoms, Treatment, Prevention & Pain Relief.' Cleveland Clinic, my.clevelandclinic.org/health/diseases/12792-sciatica.
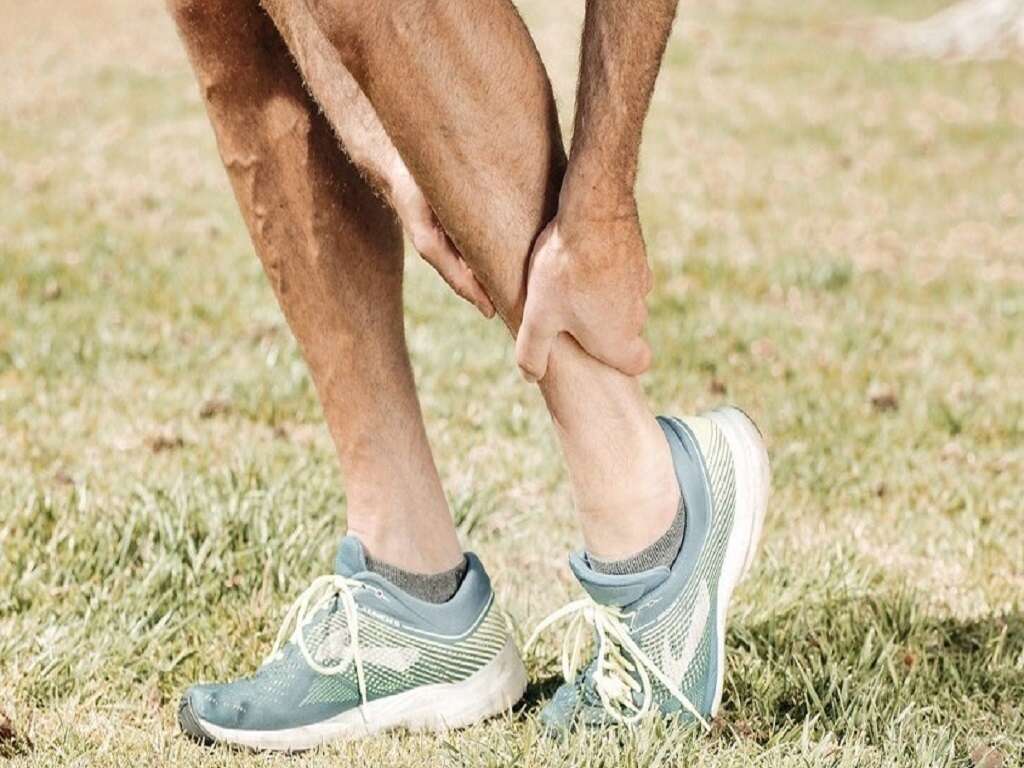
The calf muscles are located in the back of the lower leg. The gastrocnemius is the larger calf muscle, and it lies above the smaller soleus muscle. The Achilles tendon connects the calf muscles to the heel. When pain occurs in the calf, it's often due to an injury to one of these structures.1‘Calf Muscle.’ Calf Muscle | Michigan Medicine, www.uofmhealth.org/health-library/abq4737#abq4737-sec.
Sometimes calf muscle pain is related to other medical issues, and it may be the first sign of a serious problem. Depending on the cause, the calf pain may resolve with home treatment, but its important to seek medical advice if symptoms persist or get worse.2‘Calf Pain.’ Healthdirect, Healthdirect Australia, www.healthdirect.gov.au/calf-pain.

1. Leg Cramps
Sudden, severe pain in the calf muscles may be caused by a cramp. This occurs when a muscle contracts involuntarily. Intense pain may last a few seconds or a few minutes, and soreness may linger for several hours. Dehydration, mineral deficiencies and engaging in unusual exercise may cause leg cramps. Sitting for long periods of time or using certain medications may also lead to leg cramps.
People of any age may develop leg cramps, but they're more common in people over age 60 and in pregnant women. Leg cramps often occur at night. Sometimes they're a sign of a more serious condition.2‘Calf Pain.’ Healthdirect, Healthdirect Australia, www.healthdirect.gov.au/calf-pain.,3‘Leg Cramps at Night: Causes, Pain Relief & Prevention.’ Cleveland Clinic, my.clevelandclinic.org/health/diseases/14170-leg-cramps.

2. Treating and Preventing Leg Cramps
Flexing the calf muscles by pulling the toes up toward the shin may help alleviate a leg cramp. Massaging the area, walking, applying heat or cold and elevating the leg may help too. Over-the-counter pain medications may help mitigate residual pain.2‘Calf Pain.’ Healthdirect, Healthdirect Australia, www.healthdirect.gov.au/calf-pain.,3‘Leg Cramps at Night: Causes, Pain Relief & Prevention.’ Cleveland Clinic, my.clevelandclinic.org/health/diseases/14170-leg-cramps.
Stretching and exercising the legs may help keep leg cramps at bay. Remaining well hydrated and reducing caffeine and alcohol intake are helpful as well. Keeping toes relaxed and in a natural position while sleeping may also help prevent leg cramps.3‘Leg Cramps at Night: Causes, Pain Relief & Prevention.’ Cleveland Clinic, my.clevelandclinic.org/health/diseases/14170-leg-cramps.

3. Calf Muscle Injuries
Calf muscle injuries can occur as a result of overstretching one or both calf muscles. Symptoms may include sudden pain in the calf, difficulty rising up on the toes, weakness and stiffness in the calf when walking and possible bruising on the calf.2‘Calf Pain.’ Healthdirect, Healthdirect Australia, www.healthdirect.gov.au/calf-pain.
The calf muscle may be strained or torn, and this type of injury often occurs while engaging in sports. The injury may occur suddenly, or it may develop over time.4‘Calf Muscle Injury.’ Calf Muscle Injury | Michigan Medicine, www.uofmhealth.org/health-library/abq4844.

4. Treating and Preventing Muscle Injuries
Most calf muscle injuries heal with home treatment. The leg needs to rest, and applying ice for 20 minutes every hour or two can helps ease swelling. Wrapping the calf with an elastic bandage and elevating the leg may also help reduce swelling.
Taking over-the-counter pain medications may help mitigate pain. As healing progresses, activity can resume gradually. For more serious injuries, treatment may include physical therapy or surgery.4‘Calf Muscle Injury.’ Calf Muscle Injury | Michigan Medicine, www.uofmhealth.org/health-library/abq4844. Stretching before and after exercise may help prevent calf injuries.2‘Calf Pain.’ Healthdirect, Healthdirect Australia, www.healthdirect.gov.au/calf-pain.

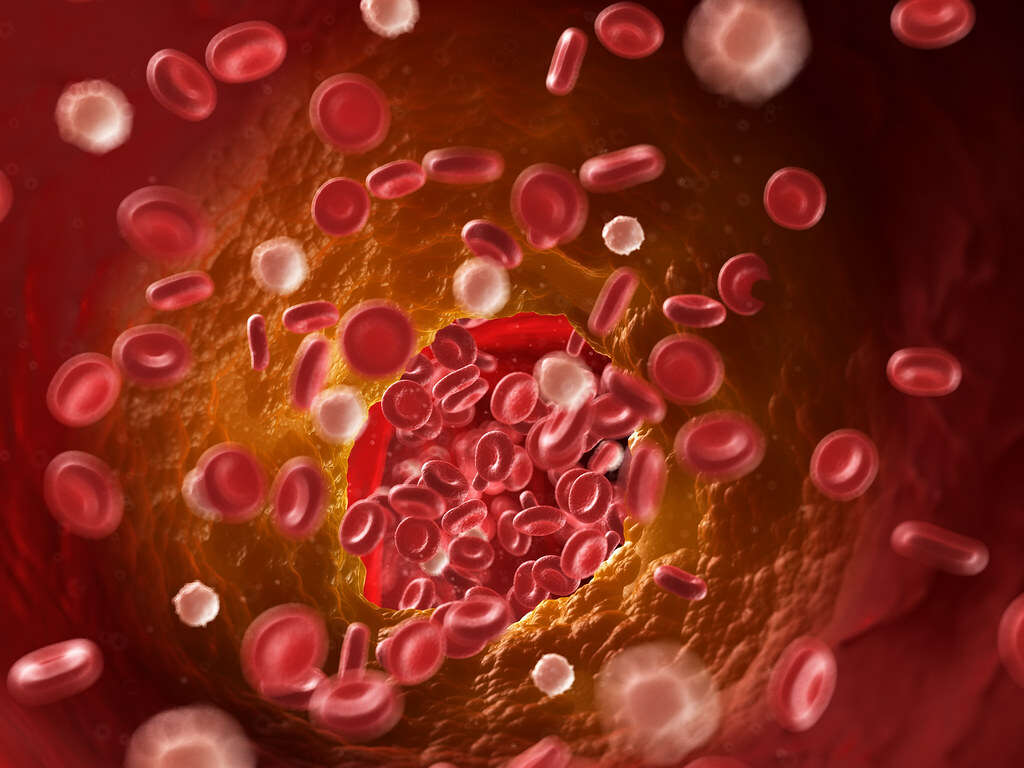
5. Blood Clot
Cramping or soreness in the calf may be a sign of something more serious, such as deep vein thrombosis. DVT occurs when a blood clot forms in a vein in the leg. If the clot breaks free, it may travel to the lungs and block blood flow.
Other symptoms of DVT include warmth, redness and swelling in the affected leg. Sitting still for long periods of time, smoking and obesity are some of the risk factors for DVT.5‘Deep Vein Thrombosis (DVT).’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 22 Dec. 2020, www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/symptoms-causes/syc-20352557.

6. Treating and Preventing Blood Clots
Treatments for DVT include wearing compression stockings, administration of oral or injected blood thinners, and intravenous medications to dissolve blood clots. A filter may also be inserted in a large vein in the abdomen to prevent blood clots from traveling to the lungs.6‘Deep Vein Thrombosis (DVT).’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 22 Dec. 2020, www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/diagnosis-treatment/drc-20352563.
Avoiding smoking and maintaining a healthy weight can help prevent the formation of blood clots in the legs. People recovering from surgery or illness should begin walking as soon as possible to prevent the development of blood clots.5‘Deep Vein Thrombosis (DVT).’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 22 Dec. 2020, www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/symptoms-causes/syc-20352557.

7. Peripheral Artery Disease
Peripheral artery disease, or PAD, is a common circulatory condition that may cause calf muscle pain while walking. This condition may develop if the arteries narrow, reducing the flow of blood to the legs. Pain or cramping may occur with activity and ease when the person is at rest.
Smoking, obesity, high blood pressure and high cholesterol levels are some of the risk factors for developing PAD. Because blood flow is restricted, PAD may lead to stroke or a heart attack.7‘Peripheral Artery Disease (PAD).’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 14 Jan. 2021, www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/symptoms-causes/syc-20350557.

8. Treating Peripheral Artery Disease
Lifestyle changes, such as quitting smoking and exercising, may help prevent and manage PAD. People may also need to take medications that help lower blood pressure, cholesterol levels and blood sugar.
An angioplasty may be necessary to widen narrowed arteries, and bypass surgery may be required to redirect blood flow around a blocked artery. Existing clots may be dissolved using an injected medication. A supervised exercise program may help the body utilize oxygen more efficiently and reduce leg pain.8‘Peripheral Artery Disease (PAD).’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 14 Jan. 2021, www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/diagnosis-treatment/drc-20350563.

9. Sciatica
Sciatica, a condition that originates in the lower back, may also cause calf pain. It occurs due to inflammation, pinching, compression or irritation of the sciatic nerve in the lower back, causing pain that radiates from the buttocks down the back of the leg. A herniated or slipped disk are common causes of sciatica.
Gentle stretching, application of ice and taking over-the-counter pain medications help alleviate discomfort. Physical therapy, prescription medications and spinal injections may also be helpful. Alternative therapies include yoga, chiropractic adjustments and acupuncture.9‘Sciatica: Causes, Symptoms, Treatment, Prevention & Pain Relief.’ Cleveland Clinic, my.clevelandclinic.org/health/diseases/12792-sciatica.
10. When To Get Medical Help For Calf Muscle Pain
A person needs immediate medical assistance if they can't walk or put weight on the leg or they have a deep cut or an exposed bone or tendon. Calf pain with swelling, redness or warmth may be signs of DVT, requiring emergency care.
A doctor's visit is necessary if the leg is weak, tingling or numb or the calf is cool or pale. If pain worsens or fails to improve with home care, or if the calf hurts while walking, medical care is indicated.2‘Calf Pain.’ Healthdirect, Healthdirect Australia, www.healthdirect.gov.au/calf-pain.