10 Symptoms of Bursitis
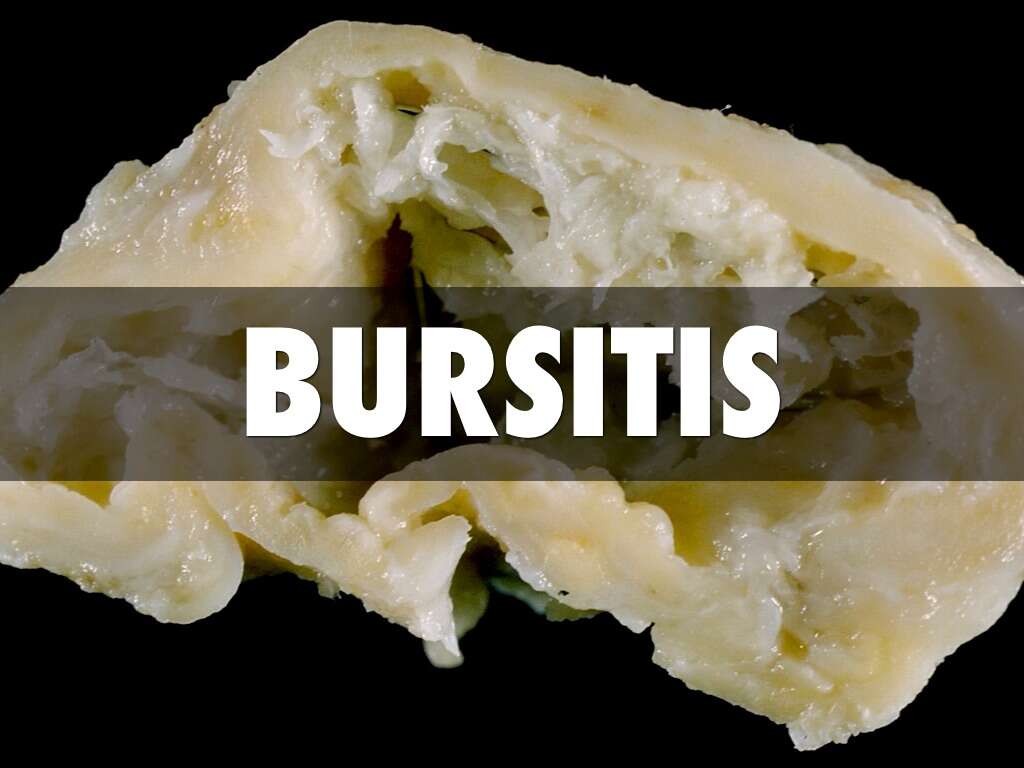
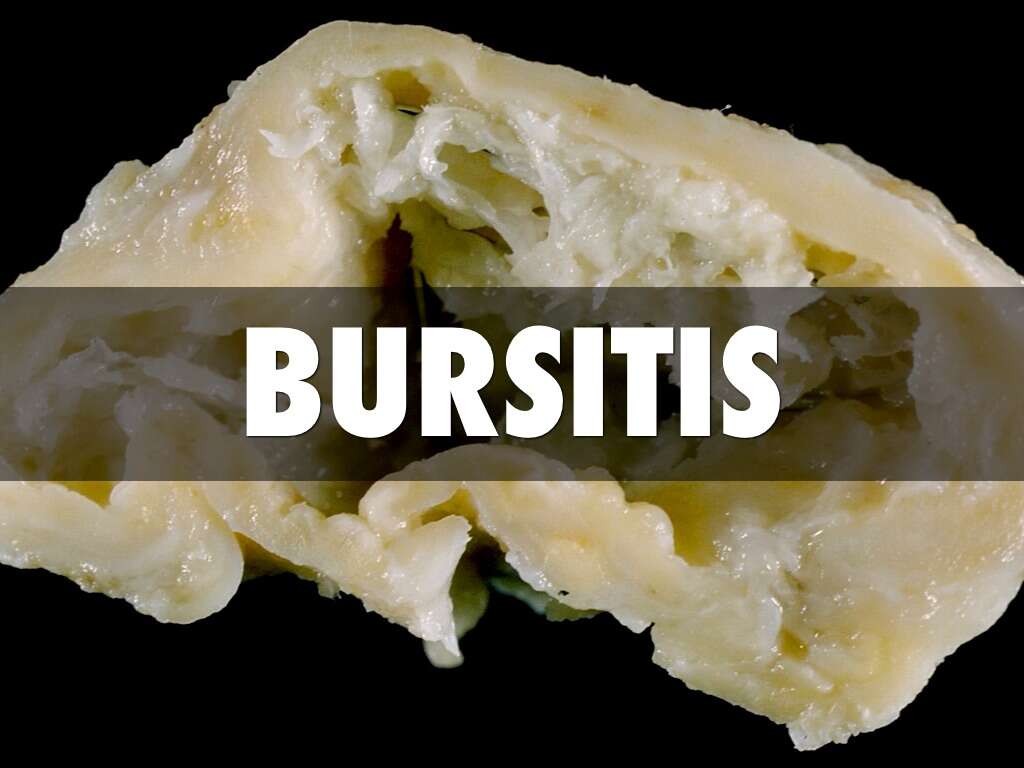
Bursae (the plural form of bursa) are small sacs of synovial fluid that can be found throughout the body. Bursae are lined with synovial membranes that function to secrete synovial lubricating fluid. Bursitis is the condition when one or more bursae are inflamed. In the human body, there are more than 150 bursae that are found in points such as tendons and muscles as they help to reduce the friction and assists them to slide across bone. A healthy bursa aids in creating a smooth and near frictionless surface that glides, making movement painless.
Once bursitis occurs, the movement that relies on the affected bursa can feel gritty and painful. Increased movements of the tendons and muscles related to the inflamed bursa further aggravates the pain and inflammation, prolonging the irritation of the bursa. This results in the affected individual not wanting to move the affected area which can lead to muscle and joint stiffness.
Some of the causes of bursitis include trauma, infection, auto-immune disorders, medication related factors, rheumatoid arthritis, gout, diabetes, scleroderma, systemic lupus erythematosus, and repetitive or overuse of the affected area. The most commonly affected areas are the shoulders, knees, and elbows. Generally, non-infected bursitis can be treated with physiotherapy, anti-inflammatory drugs, rest, ice, and elevation. Infected bursae would require more elaborate therapy.
Symptom #1: Localized tenderness
Tenderness is usually a typical symptom of bursitis. Other symptoms associated with tenderness are pain, swelling, and others. Bursitis can be accompanied by tendinitis (inflammation and irritation of tendons) surrounding the bursa. This causes focal tenderness of the surrounding inflamed and irritated tissues. It may also lead to a “pinching” pain which is commonly known as impingement.
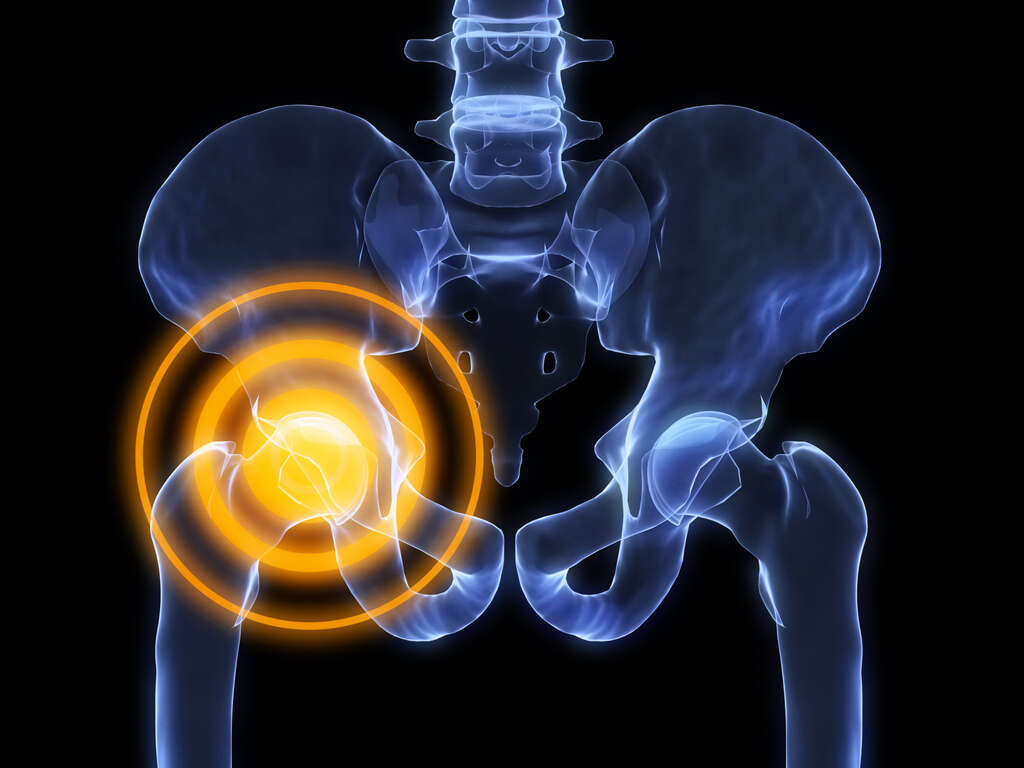
Symptom #2: Pain
When a bursa becomes inflamed, irritated, and swollen, it can lead to unwanted friction and more damage to the bursa. Bursitis can be painful as the movement causes the structures around the bursa to rub against each other without cushion or smooth gliding. The grittiness and friction cause structures such as tendons to rub against bones, or vice versa.
Trauma on the area with a bursa can also form a hematoma (a collection of blood, somewhat like a big bruise internally). The bursa may react to this and become inflamed, causing the bursa to become thickened. A thickened, irritated, and inflamed bursa can be very painful and may become chronic or long lasting.

Symptom #3: Swelling and Edema
Bursitis is a condition that can cause swelling and edema in the surrounding areas of the affected region. It refers to the swelling of the bursa which is a fluid filled sac that functions as a cushion between bones and other moving parts such as tendons or muscles.
To reduce the risk of bursitis, patients are advised not to be dormant for long durations and to cushion your body parts such as knees and elbows when there is pressure on them. It is also advisable to take breaks from repetitive activities and can be treated via rest, medication, and gentle exercises. Severe cases may require surgery.

Symptom #4: Erythema
Erythema is a word that originated from the Greek work “erythros” which translates to red. When there is erythema, there is redness of the mucous membranes or skin due to hyperemia (a term that means increased flow of blood to the superficial capillaries). It is a non-specific symptom that can occur in any condition such as trauma, skin injury, infection, inflammation, and more.
To ensure that it is indeed erythema, the redness of the affected area disappears when you apply finger pressure on the area causing blanching. In contrast to bruising or pigmentation of the skin, blanching does not occur. Generally, there is no increased warmth unless there is dilation of blood vessels under the deeper layers of the skin.

Symptom #5: Reduced Movement
Due to the pain the patient experiences from bursitis, patients are often reluctant to move the affected area in an effort to reduce the pain. In the beginning stages of bursitis, it is a good idea to reduce movement to allow the injured bursae to heal and for the pain to subside a bit. However, long periods of reduced movement can be counterintuitive as it can result in more pain, muscle atrophy, and stiff joints.
It is however advised to avoid repetitive movements that first contributed to bursitis in the first place. Patients should return to gentle exercises and stretches that are ideally guided by a physiotherapist. Future episodes and prolongation of the bursitis can be avoided with maintenance through proper exercises and healthy lifestyle choices.
Symptom #6: Stiff Joints
Another non-specific symptom that can often be attributed to old age, there are many individuals who experience stiff joints right after waking up. Lying down for a long duration can reduce the amount of synovial fluid leading to difficulty moving joints in the morning. In cases such as bursitis, pain, swelling, tenderness, and reduced movement often accompany joint stiffness.
Joint stiffness can cause movements such as walking, running, standing, or lifting objects to be difficult and painful. Bursitis is usually a temporary condition where it would usually resolve after the affected area is rested for a duration of time. Patients should keep to light activity to allow the stiffness to resolve.

Symptom #7: Warmth
In certain cases of bursitis where an infection is involved, the affected area is often warm to the touch. This means that the temperature of the skin overlaying the area of the inflamed bursa is much warmer compared to other parts of the body.
Other associated symptoms that can be noticed include redness and swelling. If you suspect septic bursitis, it is important to seek medical attention as soon as possible as the infection may involved the surrounding tendons, muscles, and joints causing septic arthritis that can be much more complicated and result in damage to the affected joints.

Symptom #8: Fever and Chills
This non-specific symptom is related to septic bursitis, a condition where the cause of the inflammation is an infectious process. Fever occurs when the body’s set point in temperature is increased as it helps the body’s immune system fight off infection better.
Chills describe a feeling of coldness when the body’s set point of temperature is increased. This can lead to shivering where the muscles in the body contract to produce heat as an effort to increase body temperature to meet the new set point of body temperature.

Symptom #9: Wounds
In septic bursitis there is usually a point of entry. The skin is one of the first lines of the body’s immune system defense as it acts as an anatomical barrier. Once there is a break in the skin, pathogens are able to invade and colonize the surrounding area. In septic bursitis, the wound may have penetrated deep enough near the bursae or damaged the bursae causing an infection.
In septic bursitis, other symptoms that may be present include pain, swelling, tenderness, fever, chills, stiffness of joints, and loss of range of movement of the affected area. you should seek medical attention as soon as possible to reduce the possible complications from a septic bursitis.
Symptom #10: Antalgic Posture
Many patients suffering from bursitis will develop and antalgic posture, meaning that they will tend to avoid pain by finding a comfortable position where the bursa is not being compressed or engaged.
This is seen often in patients with Ischiogluteal Bursitis. These patients will feel pain when sitting over long periods, so eventually, they will develop an antalgic posture.












