Cellulitis Causes, Symptoms & Treatments
Cellulitis is a skin condition where there is inflammation of the deeper layers of the skin such as the subcutaneous fat and dermal layer. While it can affect any part of the body, it usually affects the legs or face. It is caused by a bacterial infection and affects individuals of all ages, race, and gender. Cellulitis is most commonly seen in the elderly and middle age individuals. If untreated, it can spread further and involve the lymph nodes. If the infection reaches your blood stream, it can cause septicemia (or you may know it better as blood infection) leading to a life-threatening situation.
Many cases of cellulitis can be treated on an outpatient basis with no long-lasting effects. However, in some cases, admission may be needed in advanced or severe cases. If you suspect that you or someone you know have cellulitis, it is important to seek medical attention to avoid complications.

Cause #1: Bacteria
The most common bacteria types that cause cellulitis are Streptococcus and Staphylococcus. These strains are responsible for many other conditions such as strep throat, impetigo, folliculitis, abscess, and more. Both these strains are commonly found on humans and do not cause any issue until it manages to invade the deeper layers of the skin or blood stream.
Coming into contact with those who carry the bacteria can increase the risk of infection. Bacterium such as the staphylococcus strain is very hardy and can survive in the harshest environments. It can be found on surfaces such as tables, clothing, and more. Some of the other bacteria that can also cause cellulitis are methicillin resistant staphylococcus aureus (MRSA), haemophilus influenzae, clostridium, and pneumococcus species.

Cause #2: Compromised Immune System
The line of defenses of the immune system function to protect the body from being invaded by foreign pathogens. Some of these defenses are the skin barrier, tears, acidity of the stomach, white blood cells, and more. In those with a compromised immune system (elderly, those on immune suppressing medications, very young children, patients with cancer or human immunodeficiency virus infection, individuals on chemotherapy), they also have a weaker defense and have a higher risk of contracting these infections.
This allows pathogens such as streptococcus or staphylococcus to invade, colonize, and cause issues such as cellulitis. Inadequate nutrition can also be a contributing factor as proteins, vitamins, and minerals are required for optimal function of the immune system.
Cause #3: Cuts, Scratches, Wounds
As one of our primary defense systems is the skin, a break in the skin caused by a cut or scratch allows bacteria to invade. Once bacteria invade the deeper layers of the skin, it colonizes the area and multiplies causing damage to the area. If the wound becomes infected, it can be a great breeding ground for bacteria. This is the reason why any wound should be sanitized or cleaned to lower the risk of infection.
Most cases are minor, and the infection is localized to the area and only the skin. However, in severe cases, the invasion of the bacteria into the blood stream can cause joints, bones, and organs such as the heart and brain to be involved, leading to life-threatening situations.

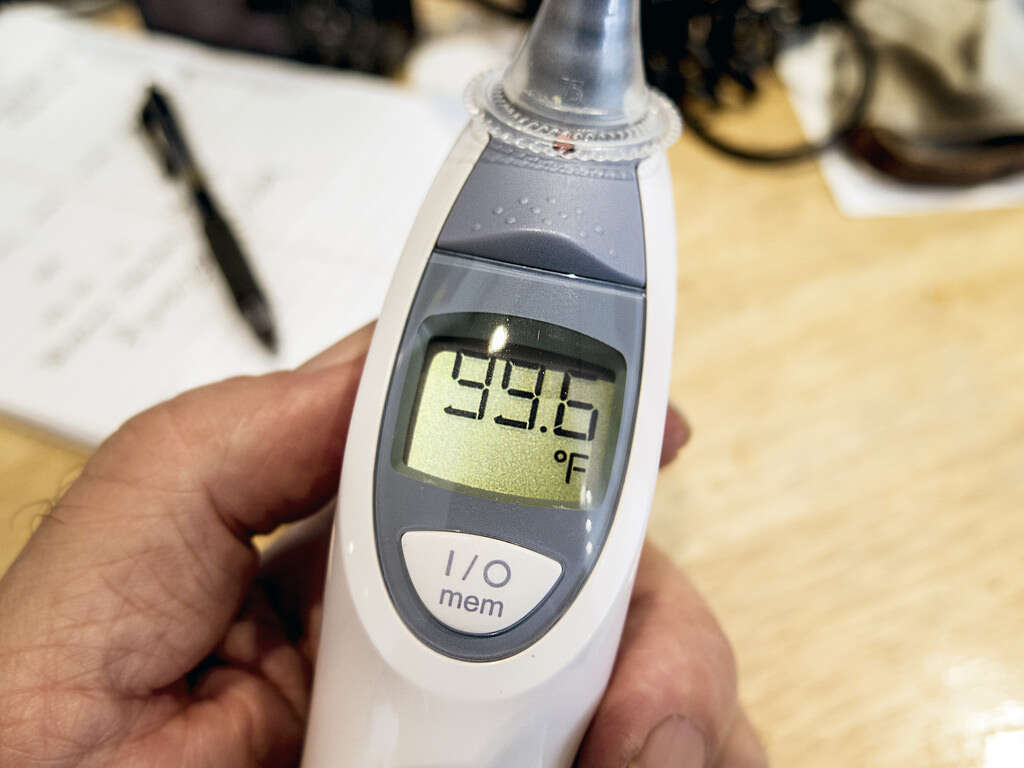
Symptom #1: Fever and Chills
Fever can occur in any infection. When the body senses that there is an invasion, one of the ways it tries to fight off the pathogen is by increasing the set point of temperature in the body. The raised temperature enhances the ability of the immune system to fight off the infection resulting in a fever.
Chills occur as the set point of body temperature increases causing the affected individual to feel cold. To help the body reach the higher temperature, shivering may occur as the repeated contraction of muscles produce heat.
Symptom #2: Redness, Swelling, Tenderness
In cellulitis, there are 4 main signs of infection: erythema (also known as redness), pain, swelling, and warmth. In most cases, the affected area does not have an elevated border. In untreated cases, this area can grow bigger signifying the spread of infection. These symptoms occur due to the presence of the bacteria and the attempt of the body to fight off the infection.
In some cases, the affected area can also look pitted or like an orange peel. There may also be blisters that are filled with fluid. These blisters can be large (called bullae) or small (called vesicles).

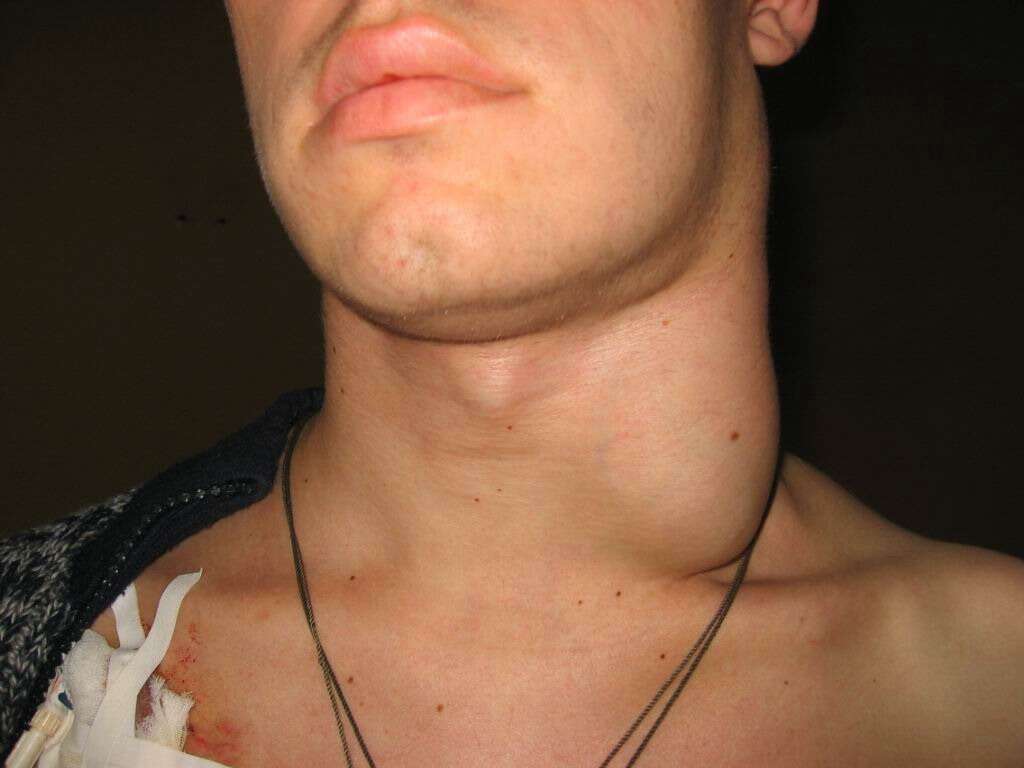
Symptom #3: Lymphadenitis and Lymphangitis
Lymphadenitis refers to the infection of one or more lymph nodes. This infection usually spreads from the infected area to a lymph node. The affected lymph node is usually painful and tender. In some cases, the skin overlying the infected lymph node may look red, inflamed and feel warm. It may be accompanied by a fever and abscesses.
Lymphangitis refers to the infection of lymphatic vessels. It occurs when the infection spreads to a lymph vessel causing red, tender, irregular, and warm streaks on the skin. It is accompanied by other symptoms such as fever, chills, tachycardia (fast heart beat), and headaches.
Treatment #1: Outpatient Care
In mild cases of cellulitis, outpatient care is sufficient. It involves oral antibiotic therapy that is selected based on the suspected organism and symptoms of cellulitis. The antibiotics can range from 7 to 14 days of treatment. In cases where there is slow response to therapy, antibiotics may be necessary until the inflammation in the affected area resolves. If there is no improvement, resistance or an alternative diagnosis should be considered.
Pain medication may also be prescribed if you have intense pain or fever. The elevation of the affected area can help reduce the swelling and pain. To help remove purulent discharge from any open wounds, cool sterile saline dressings can be useful.

Treatment #2: Intravenous Antibiotic Therapy
Intravenous antibiotic therapy is used in individuals who have severe cases of cellulitis or if they are not responsive to standard oral antibiotics. The type of intravenous antibiotic used is selected based on the suspected organism causing the infection.
If the infection occurs in a hospitalized individual, community acquired methicillin resistant staphylococcus aureus (CA-MRSA) should be suspected. Other patients who may require intravenous antibiotic therapy are patients with weakened immune systems, those with facial cellulitis and patients with a clinically significant condition such as heart, liver, or kidney failure.

Treatment #3: Surgical Examination and Drainage
In severe and advance cases of cellulitis, there can be crepitus (which means that there is air underneath the skin), circumferential cellulitis (cellulitis in a pattern that surrounds the entire limb such as around the calf), necrotic looking skin, abscess, and severe pain. Surgery and drainage may be required in these cases to debride the dead skin tissue and to allow the rest of the infected area to heal better.
In circumferential cellulitis, surgical decompression may be needed in case of compartment syndrome (a painful condition where the pressure within the muscles build up cutting off the blood supply that carries oxygen and nutrients). Abscesses should be drained to allow healing.












