What Is MS?
MS (multiple sclerosis) is a condition where the insulating covers of nerve cells are damaged. This process is known as demyelination. This damage negatively affects the ability of the nerve cells to communicate, leading in various issues. It is a condition that can produce significant disability in more than 30% of patients within 20 to 25 years.
The hallmark of MS would the episodes of symptoms that occur periodically with months or years without symptoms. This means that between the “attacks” or “episodes,” the symptoms can disappear completely despite having permanent neurological issues especially when the disease is advanced.
1. Pathophysiology
In MS, the 3 main characteristics are the destruction of myelin sheaths, inflammation, and the presence of plaques in the central nervous system. This condition is believed to be due to a combination of environmental and genetics causing the individual’s own immune system to attack their nervous system. The plaques are most commonly found to affect the spinal cord, basal ganglia, optic nerve, brain stem, and white matter tracts that are close to the lateral ventricles. Since the condition affects the oligodendrocytes that are responsible for the myelin sheath, the loss of this layer results in the inability of the neuron to conduct electrical signals. The inflammatory process in MS is caused by T-cells that are a type of lymphocyte (white blood cell) that in turn, attack the myelin sheath.

2. Etiology
Since the cause of MS is unknown, there are several hypotheses regarding what may contribute to the development of the condition. Studies on twins with MS have suggested that there may be a genetic factor for MS. Individuals with first-degree family members with MS have 7 times higher risk compared to the general population.
It is also observed that MS is less common among individuals who live nearer to the equatorial regions of the world. Another theory would be regarding a viral infection that may activate the T-cells that attack the myelin sheath. The development of MS has been associated with an Epstein Barr virus infection. Other theories include low vitamin D levels and chronic cerebrospinal venous insufficiency.
3. Epidemiology
In the United States, it has been estimated that the prevalence of MS ranges from 58 to 95 per 100,000 individuals. Per the National Multiple Sclerosis Society, as many as 400,000 individuals are affected. However, misdiagnosis is common. MS is more common among women and is usually diagnosed at the ages of 15 to 45 years old.
However, it can occur at any age. Globally, about 2.1 million individuals have MS with lower rates among the Japanese, Chinese, and African blacks while being higher among Palestinians, Sardinians, and Parsis. MS is the commonest immune mediated condition that affects the central nervous system.

4. Patient History
The “attacks” or “episodes” of multiple sclerosis can occur several months or years apart. The presentation of MS can vary. Some of the issues patients experience include sensory loss, paresthesia, muscle cramping, spasticity, bladder dysfunction, sexual dysfunction, bowel dysfunction, and nystagmus.
Others can also experience intention tremor, dysarthria, bilateral facial weakness, trigeminal neuralgia, optic neuritis, heat intolerance, diplopia, fatigue, dizziness, lack of sleep, pain, depression, aphasia, dysphasia, seizures, cognitive difficulties (memory, attention span, concentration, judgment, visual perception, problem-solving, abstract reasoning, executive function), ataxia, akinesia, and pruritus.
5. Categories
MS can be categorized based on the frequency of relapses, lesion development, and time to disease progression. It can therefore be divided into relapsing remitting MS (RRMS) where there are recurrent attacks where neurologic deficits appear in different parts and resolve in a short duration, secondary progressive MS (SPMS) where there is progressive neurologic decline without periods of remission, primary progressive MS (PPMS) where there is no remission and progression of disability from the onset, and clinically isolated syndrome (CIS) where there is an attack suggestive of demyelination but does not fulfill the criteria for MS.
It is estimated that 30% to 70% of individuals with CIS eventually develop MS.
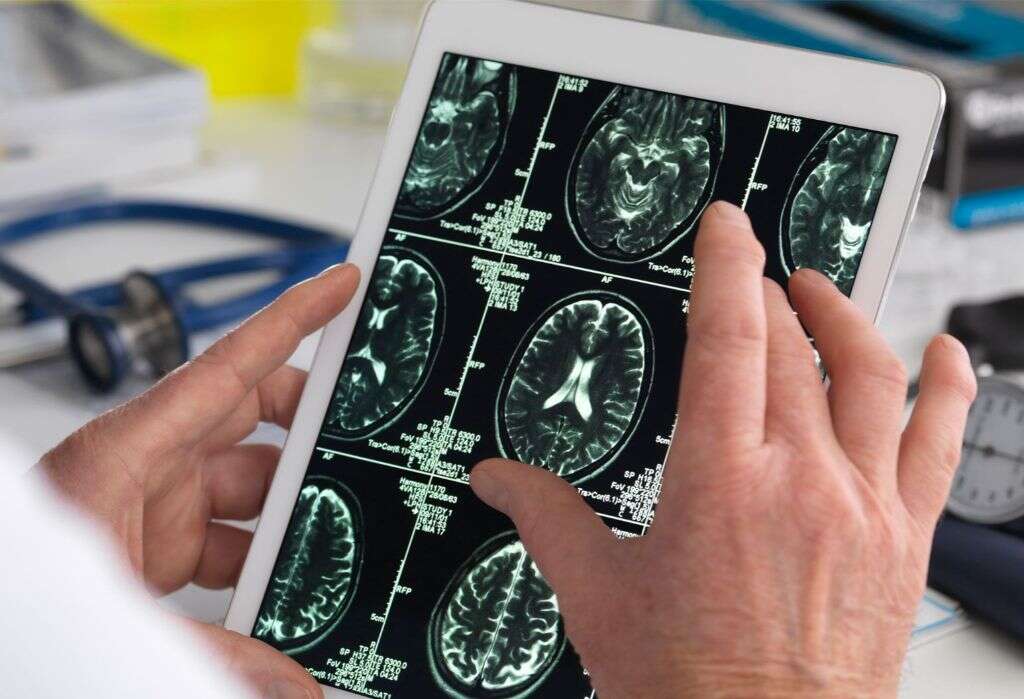
6. Diagnosis
MS can generally be diagnosed based on the patients signs and symptoms along with supporting investigations such as blood tests and medical imaging. In the early stages of the disease, it can be difficult as it can resemble many other conditions. The McDonald criteria is the commonest method used for diagnosis.
Some investigations that may be beneficial are neuroimaging, magnetic resonance imaging (MRI) of the brain, and analysis of cerebrospinal fluid (CSF). In the MRI, gadolinium can be administered to highlight plaques. The CSF analysis can confirm the presence of chronic inflammation due to the presence of oligoclonal bands of IgG found in 75% to 85% of MS patients. The results of blood tests from MS patients are generally normal.

7. Treatment
Despite not having a cure, there are several therapies that may be helpful. The main goal is to return function after an episode, prevention of new episodes, and decreasing disability. In an acute setting, intravenous or oral corticosteroids can be beneficial.
The use of disease-modifying treatments such as alemtuzumab, ocrelizumab, and rituximab can slow disease progression. Stem cell transplant shave also been suggested to have potential benefits. Physical Therapy and Occupational Therapy are a key part to treatment. Many MS patients may use alternative or complementary medicine, although the evidence for effectiveness is often weak or absent. Some treatments with unproven benefit include vitamin D supplementation, yoga, hyperbaric oxygen therapy, herbal medicine, acupuncture, reflexology, and mindfulness.

8. Symptom Management
Symptom management is an essential part of managing MS. This can be done via both pharmacological and nonpharmacological means. As mentioned above, physical therapy can be a valuable resource for the physical symptoms of MS.
For those with cognitive dysfunction, supportive therapy along with speech and occupational therapy may be beneficial. For those with depression, selective serotonin reuptake inhibitors and tricyclic depressants may be beneficial. As fatigue is one of the most common symptoms that greatly affects patients, medications such as amantadine, methylphenidate, and modafinil may be helpful. For pain, tricyclic antidepressants, anticonvulsants, and nonsteroidal anti-inflammatory drugs (NSAIDs) can also be prescribed. Patients should avoid hours of the day that are hot and use air conditioning to deal with heat intolerance. Spasticity can be managed using baclofen, benzodiazepines, and gabapentin. Other issues that should be addressed include bladder issues, impaired ambulation, bowel issues, sexual dysfunction, optic neuritis, and tremors. Symptom management is crucial as it helps increase the quality of life for patients.

9. Prognosis
Left untreated, it is estimated that more than 30% of MS patients will eventually develop significant physical disability within 20 to 25 years. There are several research trials where disease modifying agents have helped to decrease disease and disability progression but it is still unknown if these effects can be maintained over a longer period.
It has been observed that male patients who have primary progressive MS have the worst prognosis. This is due to the less favorable response to treatment with rapid progression to disability. Patients with MS only have a slightly shortened life expectancy with the survival rate being linked to disability. Death is generally due to complications such as renal or pulmonary causes.

10. Patient Education
Patients should be educated regarding their medications, uses, doses, and possible side effects. Along with their family members and caregivers, they should be taught regarding management of pain, spasticity, fatigue, bladder issues, bowel issues, and sexual function.
For those with advanced disease, caregivers should be trained regarding transfer techniques, urinary collection devices, bowel programs, and managing skin integrity. Due to high probability of falling, patients should also be taught about fall prevention. They should be made aware about the availability of community agencies, support groups, and professional organizations that are dedicated to MS. The National Multiple Sclerosis Society is recommended for resources, research, hypotheses, and education.