What Is Mania?
Mania, manic syndrome, or a manic episode refers to the state of mind where it is abnormally elevated. By definition, this state should last at least one week where an unusually irritable mood, expansive, or elevated mood exists. Individuals going through this state may describe it as “being on top of the world” as they feel very euphoric.
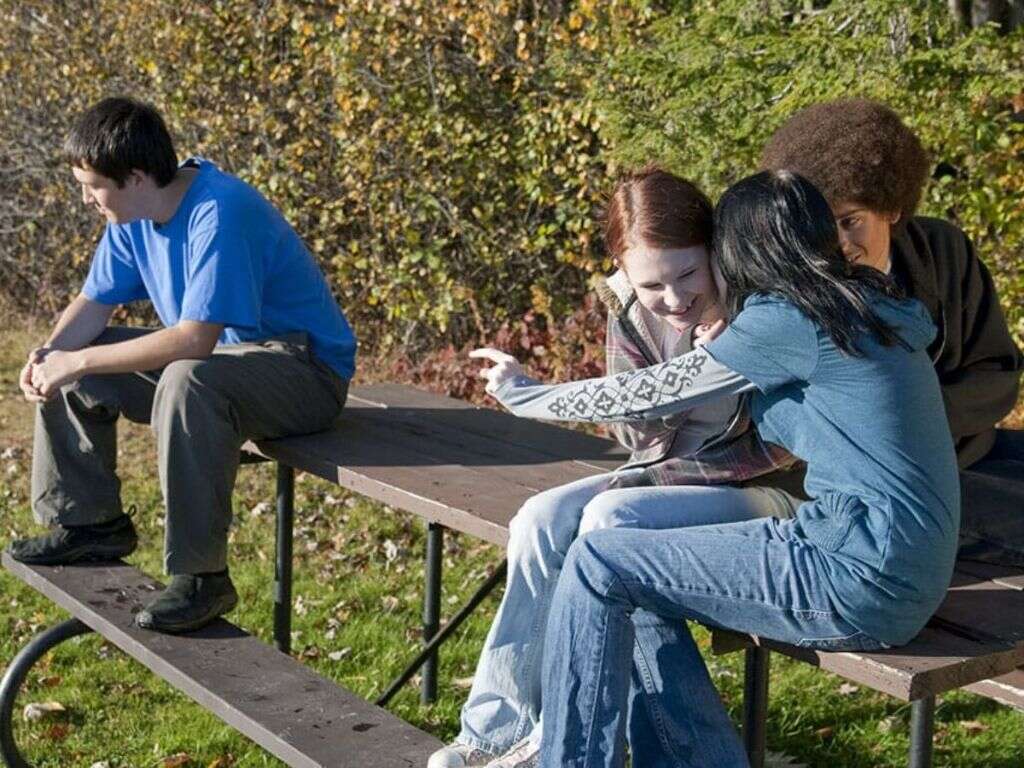
Those who are experiencing mania are usually abnormally engaged in goal-directed activities. There can be extreme optimism. In some cases, the mood can be more irritable, especially if they are denied of their wishes. This change is usually observable by friends and family. It should be severe enough to cause issues or impairment with their daily routines or family and friends. This article will be discussing bipolar disorder as a cause of mania.

1. Causes
Mania is a state that can be seen in various disorders. However, most cases of mania occur with an underlying diagnosis of bipolar disorder. It can also occur in schizoaffective disorder, multiple sclerosis, other medical conditions (encephalitis, brain injury, stroke, dementia, lupus), substance abuse (cocaine, caffeine), or as a side effect of medications (such as prednisone and antidepressants).
Mania can also occur due to a combination of factors such as high levels of stress, lack of sleep, changes in sleep patterns, seasonal changes (mania and hypomania are more common during spring), significant life event (divorce, moving, loss of a loved one), childbirth, trauma, and abuse.

2. What Is Hypomania?
The term “hypomania” translates into “less than mania.” It is a milder form of mania that does not impact or decrease the patient’s quality of life. It can be beneficial as it increases creativity and productivity. The signs and symptoms of hypomania are similar to mania where there is reduced need to sleep, increased metabolism, and more goal-oriented behavior.
Although hypomania can be beneficial due to the higher energy and elevated mood, mania can result in many undesirable consequences in terms of relationship and other aspects of personal life. Just like an individual with mania, a person with hypomania can appear to be outgoing, engaging, and excessively optimistic.

3. Definition
The American Psychiatric Association has a diagnostic manual that defines mania as a “distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased activity or energy, lasting at least one week and present most of the day, nearly every day.” It should not be caused by any underlying medical condition or drugs or medication.
The mania patient should also be causing obvious issues in social relationships, activities, and work, requires hospital admission to protect themselves or their loved ones, or is experiencing psychosis. If there is concurrent depression, it is a mixed episode, while hypomania is a lesser form of mania.

4. Signs and Symptoms
Some of the signs and symptoms of mania include increased goal-oriented activities, elevated energy, increased sense of self or grandiosity, more talkative than usual (even with strangers), and pressured, rapid speech.
Also there is a reduced need for sleep or insomnia, flight of ideas (can be observed in speech where the patient has many ideas and flits from one to another), easily distracted, hypersexuality (more promiscuous behavior or having sex with multiple partners in a short duration), impulsiveness (shopping spree, gambling, multiple business ventures), and possible irritability and quick to anger (especially if denied of their wishes). There can also be physical symptoms such as weight loss, sweating, and pacing.

5. Bipolar Disorder
The majority of mania cases occur in individuals with an underlying diagnosis of bipolar disorder. Previously known as manic depression disorder, it is a condition that causes the individual to have periods of abnormally elevated mood and depression.
The risk of suicide and self-harm among patients with bipolar disorder is higher compared to the normal population. It can be categorized into two main groups. In bipolar type I, there is alternating depression and mania, while in bipolar type II, the individual alternates between depression and hypomania. The combined prevalence of bipolar type I and II has been estimated to be 1.8% to 4%. It is a debilitating disease that can have many negative impacts on the quality of life.

6. Statistics
In the United States, the lifetime prevalence of bipolar disorder including the subsyndromal forms is estimated to range from 0.9% to 2.1% with 1% for bipolar type I and 1.1% for bipolar type II. Worldwide, the prevalence is about 0.3% to 1.5% with 0.6% for bipolar I and 0.4% for bipolar II.
The age of onset ranges from childhood to 50 years old with the average age at about 21 years old. Most cases begin around the ages between 15 to 19 years old and the second most frequent range is between 20 to 24 years old. The onset of mania for those above the age of 50 should lead to additional tests to rule out neurological or medical disorders such as a stroke. Bipolar disorder occurs equally in both genders.

7. Diagnosis
The diagnosis of bipolar disorder can be achieved based on the signs and symptoms the patient has experienced. Interviewing a family member or friend can also be beneficial.
Investigations (complete blood count, fasting glucose, erythrocyte sedimentation rate, electrolytes, proteins, biomarkers, thyroid hormones, creatinine, blood urea nitrogen, liver function tests, screening for alcohol or substance abuse) and medical imaging (magnetic resonance imaging, electrocardiography, electroencephalography) can be used to rule out other conditions such as epilepsy, acquired immunodeficiency syndrome (AIDS), cyclothymic disorder, circadian rhythm desynchronization, substance abuse disorders (hallucinogens, amphetamines, cocaine, alcohol, opiates), and multiple personality disorder. A review of the patient’s medications can also be beneficial as some medications (like antidepressants, captopril, corticosteroids, bromocriptine, levodopa, and more) can also be the cause of mania.

8. Treatment and Management
The treatment and management of bipolar disorder depends on the phase and severity of the disease. If the patient is a danger to themselves or others, has severe psychotic symptoms, or has loss of control, the patient may be admitted for inpatient management.
During mania, medications such as antipsychotics (olanzapine, risperidone, quetiapine), valproate, lithium, and benzodiazepines can be prescribed. However, the specific type of medication will depend on the symptoms the patient is having. In the depressive state, a combination of antidepressants and a mood stabilizer may be prescribed. Electroconvulsive therapy can also be useful when rapid treatment is required or when there are no improvements with medication.

9. Prognosis
Bipolar disorder is a condition that results in significant morbidity and mortality rates. A study in the early 1990s in the United States estimated that the lost of productivity resulted in about $15.5 billion annual loss; 25% to 50% of bipolar patients attempt suicide with 11% being successful.
After the first manic episode, 40% to 50% go on to experience another episode of mania within the first two years. Only 50% to 60% of bipolar patients on lithium are able to control their symptoms. Some factors that suggest a worse prognosis are psychotic features, substance abuse, depression, and poor job history. Factors that suggest a better prognosis are older age of onset, short episodes of mania, few psychotic symptoms, few suicidal thoughts, and few medical issues.

10. Patient Education
One of the most important aspects of management is patient education. Education should not only be directed at the patient but also involve their family members and those who are part of their support system. There is evidence showing that educational efforts increases the knowledge, quality of life, and patient compliance.
Patient education should include explanation of the disease, the importance of compliance to medication, how to monitor their symptoms, and early warning signs. It should also help patients identify potential stressors and how to handle relapses. Patients and family members may also benefit from a support group as individual stories can help them learn and cope with the disease.