What Is H. Pylori?
Helicobacter pylori (H. pylori) was previously known as Campylobacter pylori. It is a Gram negative bacteria (according to a method of staining used to classify bacteria) that is usually found in the stomach. It is a ubiquitous organism that can be found in as many as 50% of the global population. First identified by Australian doctors Robin Warren and Barry Marshall in 1982, they observed that it was present in individuals with gastric ulcers and chronic gastritis.
H. pylori has been linked to the development of gastric ulcers, duodenal ulcers, and stomach cancer. However, as many as 80% of infected individuals are asymptomatic. The infection is especially common in developing countries. Due to the helical shape of the bacteria, it is thought to have evolved into this shape to enable it to penetrate the mucoid lining of the stomach. The commonest route of infection would be oral to oral or fecal to oral contact.

1. Pathophysiology
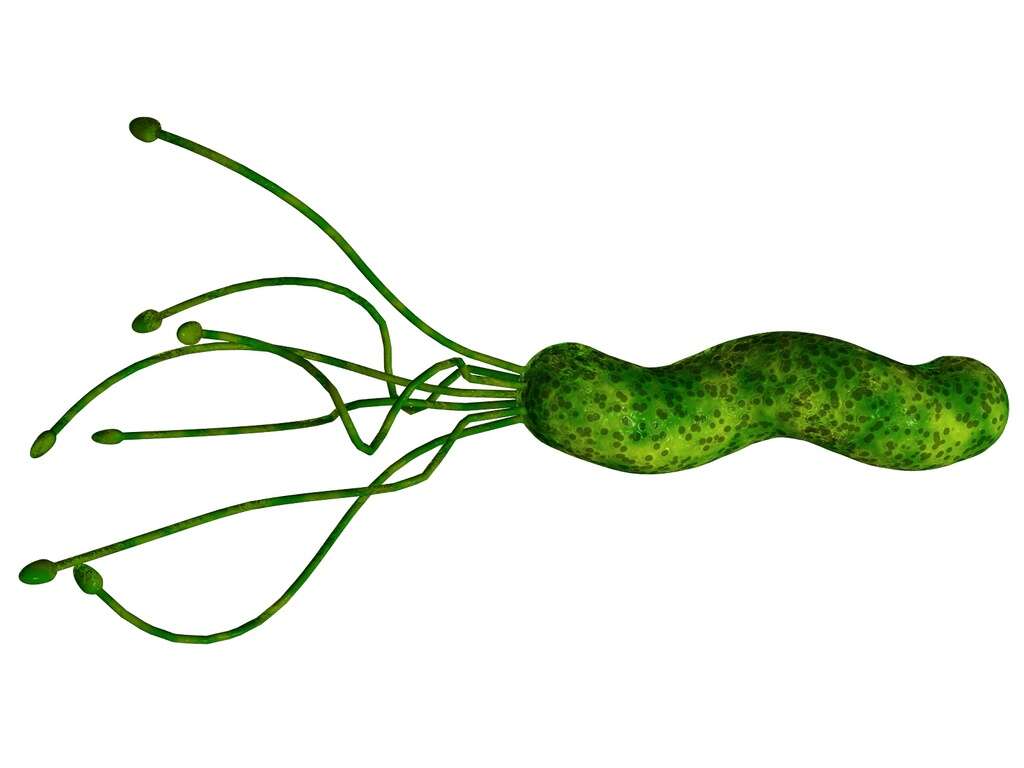
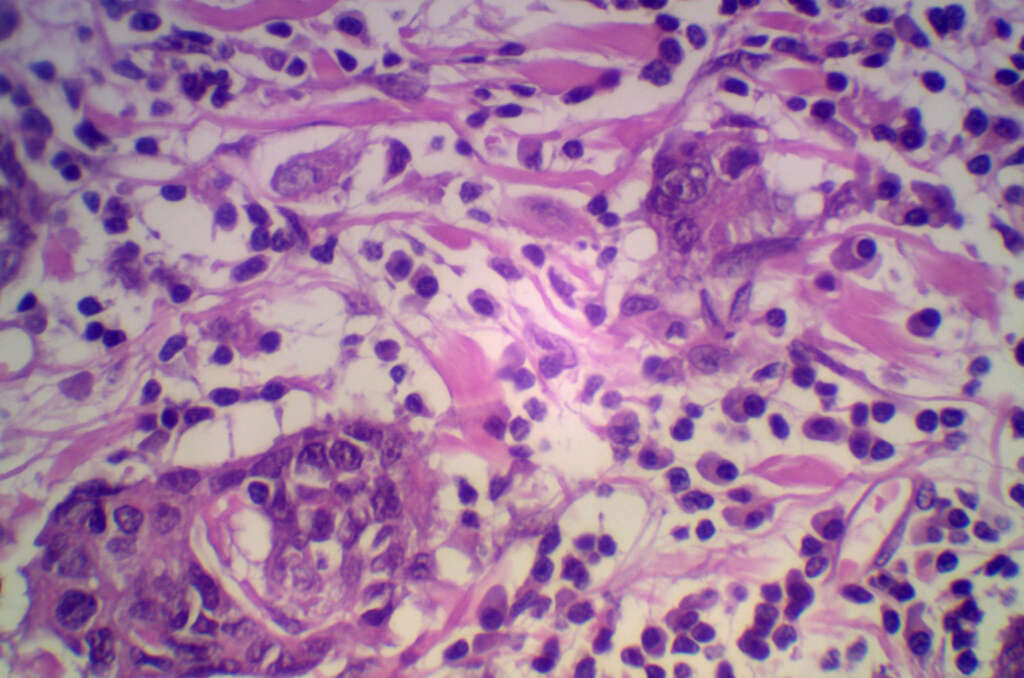
Since the most common route of infection is mouth to mouth or stool to mouth contact, a primary role in transmission is seen among parents and siblings. In a susceptible individual, the infection leads to chronic active gastritis that can result in duodenal and gastric ulcers and cancer. H. pylori causes striking infiltration of the gastric lining or epithelium and the underlying lamina propria by cells that belong to the immune system (i.e. neutrophils, macrophages, lymphocytes). The bacteria use its flagella (whip-like structure that acts a propeller) to burrow into the mucus lining as it is less acidic. The infection also results in the production of toxins that harm cells (cytotoxins) and can cause inflammation. This means colonization of the stomach by the bacteria can result in inflammation and chronic gastritis.

2. Epidemiology
H. pylori infection has been linked to race. For example, 60% of cases were observed to occur in Hispanics while only 29% occur in Caucasians. Internationally, it is a common organism and can be found in up to 50% of the population. In patients with peptic ulcer disease, as many as 90% have found to have H. pylori infection.
However, there are fewer than 15% of individuals with H. pylori infection that experience peptic ulcer disease. Although both genders are affected equally, females have a higher incidence of reinfection compared to males. The infection can occur at any age and is acquired most frequently during childhood.

3. Patient History and Physical Examination
Patients with H. pylori infection are usually asymptomatic. No specific symptoms can be attributed to the disease. However, when the infection results in chronic gastritis, patients can experience acute abdominal pain, nausea, vomiting, heartburn, and foul breath (halitosis).
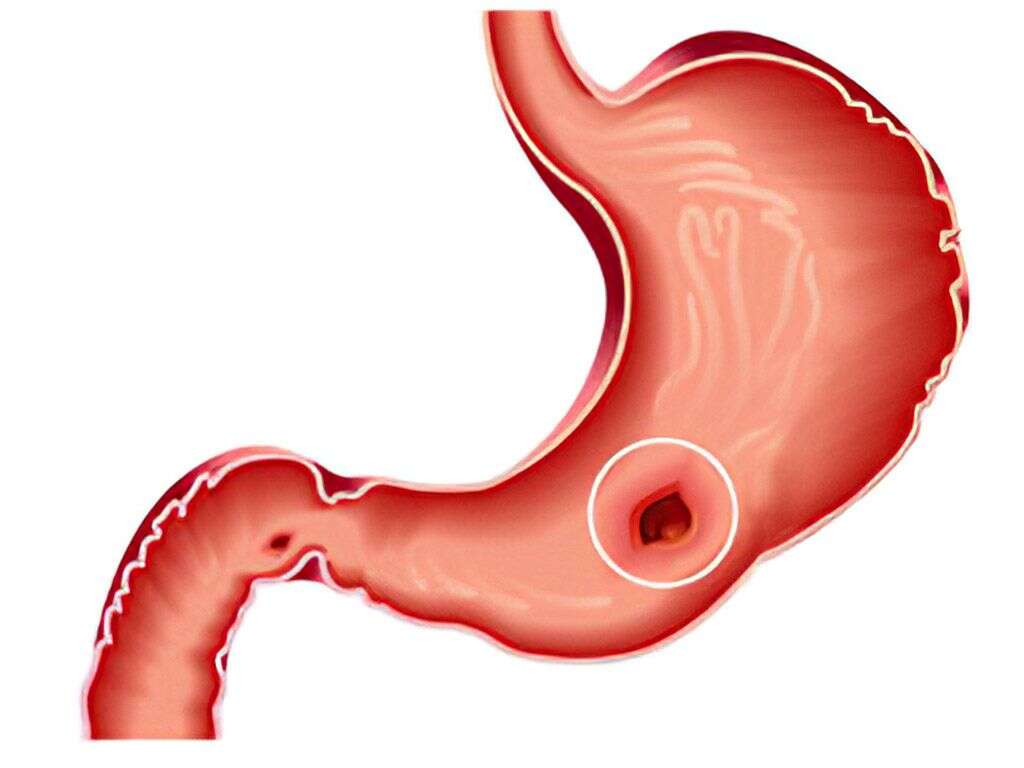
Furthermore, chronic gastritis may lead to peptic ulcers. In gastric or duodenal ulcers, pain in the upper half of the abdomen (epigastrium) can occur. Epigastric pain is more likely to occur when there is an empty stomach (i.e. early hours of the morning or between meals). Moreover, if hemorrhaging occurs, it can result in vomiting of blood or dark feces (due to presence of digested blood components). Those with the infection have an increased risk of peptic ulcers and gastric cancer (adenocarcimoma).

4. Microbiology
H. pylori is a helix-shaped Gram negative bacterium that can be demonstrated using different stains. This bacterium has the ability to form biofilms (thin film that enables adhesion to surfaces) and has four to six flagella, making it extremely motile.
Since it is microaerophilic, it requires a minimum level of oxygen for growth. It also contains an enzyme called hydrogenase that produces energy through molecular hydrogen oxidization due to intestinal bacteria. The bacterium also produces catalase, urease, and oxidase.

5. Lab Tests
Some of the noninvasive diagnostic studies include the fecal antigen test, which is based on monoclonal antibody immunochromatography. Moreover, the carbon 13 urea breath test for H. pylori infection is based on the detection of the products when the bacterium splits urea. In this test, patients drink a beverage (urea) labeled with a carbon isotope.
After a while, the concentration is measured in the breath. Although expensive, it is becoming increasingly available. Also, the H. pylori serology has a high sensitivity and specificity. It is based on the quantity of immunoglobulin G antibodies against H. pylori. It is a good test to help detect H. pylori infection among newly infected patients but not for follow-up cases. For areas with a high resistance rate against clarithromycin and metronidazole, using culture testing for H. pylori can also be beneficial.

6. Imaging and Histology
Although imaging is generally not helpful for the diagnosis of the H. pylori infection, it can be useful among those with complicated disease such as gastric cancer, ulcers, and MALT lymphoma. On the other hand, advanced endoscopy is instrumental for the accurate diagnosis of gastritis, intestinal metaplasia, and atrophic mucosa.
In those with prior peptic ulcer disease, an esophagogastroduodenoscopy (EGD) can be performed. This helps physicians to view the condition of the mucosal lining of the duodenum and stomach, and to obtain biopsy specimens from both the body and antrum of the stomach. Tissue biopsy is required for histologic evaluation of gastritis.

7. Disease Process
While a staging system for the infection does not really exist, there are some phases of the disease that can be well described. It begins with chronic gastritis or the inflammation of the stomach lining that appears slowly over time. This is then followed by atrophic gastritis which refers to the loss of glandular cells that are part of the gastric mucosa.
Experts have found that the extent and severity of atrophic gastritis is correlated with the risk of gastric cancer. Later, intestinal metaplasia will follow. This involves the replacement of the atrophied gastric tissue with intestinal-type lining, glands and fibrous tissue. This transition is considered to be a premalignant change, which means that under persistent stress it can progress to dysplasia and eventually result in gastric adenocarcinoma. Although a very slow process, the prognosis is poor. Furthermore, there is another type of malignancy associated with H pylori infection. MALToma is a form of lymphoma that involves the lymphoid tissue associated to mucosal sites (i.e. gastric mucosa). In these patients, EGD and ultrasonography should be considered to ensure a precise staging of the disease.

8. Medication
Only H. pylori positive patients should be treated. These patients should be educated regarding the importance of completing the course of medication and potential adverse effects. When selecting the regimen for the patient, it is important to consider the potential of antibiotic resistance.
Regimens recommended for the treatment of H. pylori infection are triple therapies with reported cure rates ranging from 85% to 90%. Due to the increasing resistance, there has also been an increase in failure rates of standard therapy. Triple therapies should be administered for 10 to 14 days. For patients without complications, no dietary or physical activity limitations are required. A urea breath test can be considered 4 to 12 weeks after treatment for monitoring purposes.

9. Prognosis
The prognosis for individuals with H. pylori infection is excellent even for those with complications. However, once there is development of gastric carcinoma or esophageal cancer, the prognosis becomes poor. The mortality rate from H. pylori infection is usually due to complications such as ulcer perforation or mucosa associated lymphoid tissue (MALT) lymphoma.
The most severe consequence of the infection is gastric adenocarcinoma. The MALT lymphoma can be treated with eradication therapy of H. pylori and results in a better prognosis than gastric adenocarcinoma. Patients with a high risk of gastric cancer that test positive for H. pylori infection should begin eradication therapy. However, patients should be familiar with the adverse effects of the therapy and the importance of the full regimen to prevent resistance and relapse.
10. Prevention
H. pylori plays a major role in some diseases that occur in the upper gastrointestinal tract. Due to the increasing resistance to antibiotics, there is a need for new therapeutic strategies, that may include vaccination as a method of prevention.
Specifically, in patients with high risk for developing gastric cancer (i.e. history of gastric cancer in a first-degree relative), even if asymptomatic, proper screening for H pylori infection is recommended. Also, patients with precancerous gastric lesions should be considered for diagnosis and treatment of H pylori infection. If you experience several of the symptoms described in this article, you can consult your gastroenterologist on whether H pylori screening is appropriate for you.