What Is Gastroparesis?
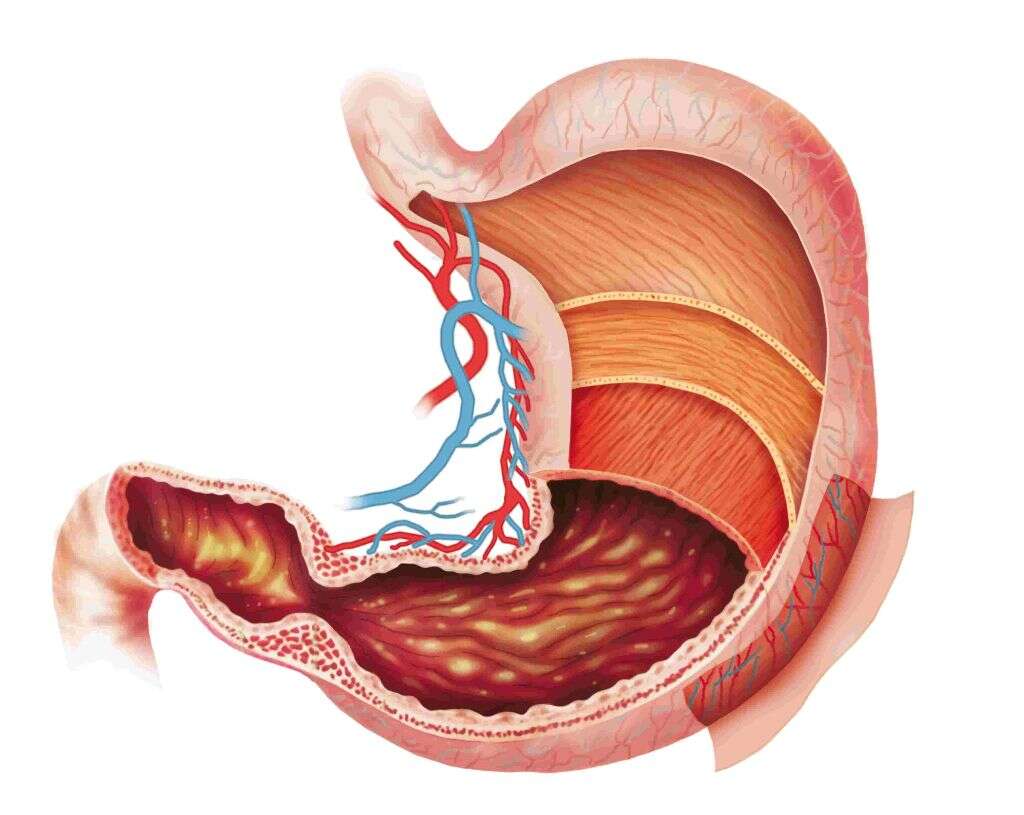
Gastroparesis is a condition that prevents food from moving through your stomach as quickly as it should. The muscles within the stomach do not contract normally. Instead, they move more slowly or don’t work at all. This leaves food sitting in your stomach for longer than it should.
The term gastroparesis means “stomach paralysis.” In a normal stomach, your muscles work to pulverize ingested food, which then is able to move down into the small intestines. When the food doesn’t get crushed, it can’t continue on.
1. Causes of Gastroparesis
It isn’t always clear what causes gastroparesis in any given person; however, there are a number of known factors that can result in the condition. Diabetes is the leading cause, but infections and autoimmune and endocrine disorders, as well as neuromuscular diseases and connective tissue disorders, are also potential causes.
In addition to physiological causes, there are several other possible factors that can lead to developing gastroparesis. Eating disorders can result in slow gastric emptying, though the condition is often remedied when normal eating patterns are again established. Some psychological disorders are associated with gastroparesis, as are some medications and medical procedures.
2. Risks Factors for Gastroparesis
More women develop gastroparesis than men. If you have diabetes, your risk of acquiring the condition is high. People who have hypothyroidism, Parkinson’s or scleroderma also face the possibility of getting it.
Undergoing surgery on your abdomen or esophagus carries the potential for getting gastroparesis as a result. Other risk factors include contracting a viral infection or taking narcotic pain medications.

3. Symptoms of Gastroparesis
This condition is associated with a number of symptoms that are caused by having too much food sitting in your stomach for too long. Heartburn and indigestion are common in people with gastroparesis, as are nausea and vomiting. People also tend to feel full after consuming very little food. Abdominal bloating or pain, erratic blood sugar levels, loss of appetite, weight loss and malnutrition are also possible.
Some of the symptoms of gastroparesis are common to other conditions. If you are experiencing any of the symptoms with regularity, it is important to contact your doctor for a correct diagnosis. It is also possible to have gastroparesis without showing any of the above symptoms.

4. Complications from Gastroparesis
Complications from gastroparesis are not uncommon. For people who have diabetes, controlling blood sugar becomes particularly difficult, as levels tend to spike when the food finally moves into the intestines. Dehydration is another concern due to the inability to keep liquids down.
When your body is unable to properly digest food, getting enough nutrients is a challenge. As a result, gastroparesis can lead to malnutrition. Food that sits in your stomach too long can also harden into what is known as a bezoar, which further inhibits the passage of food into the small intestines. Furthermore, bacterial infections can arise from the fermentation of undigested food.
5. Diagnosis of Gastroparesis
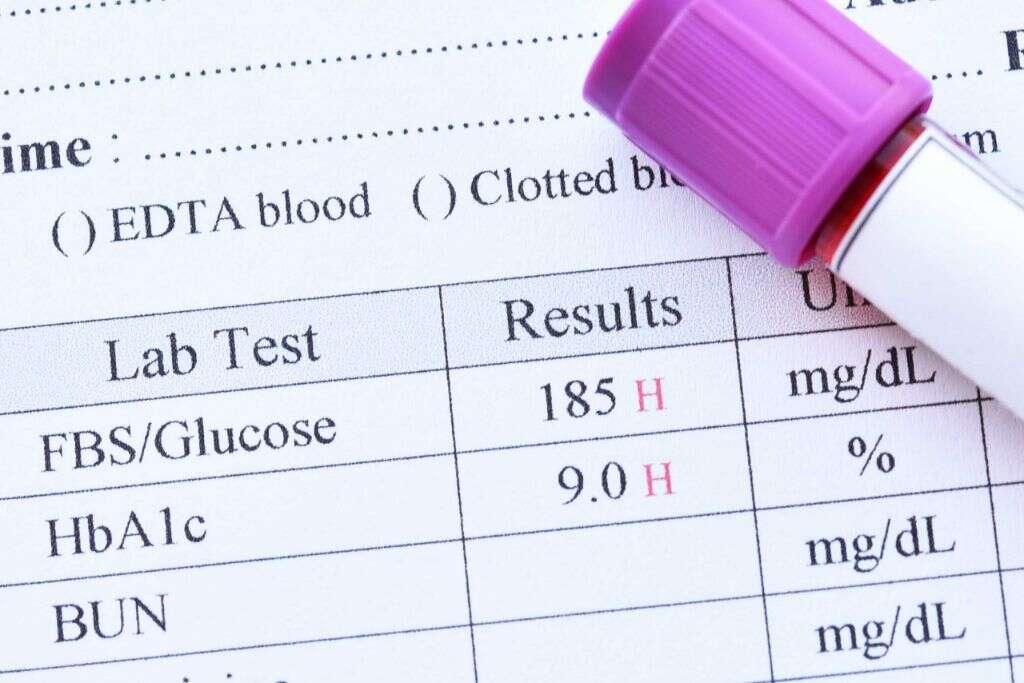
There are several means by which doctors diagnose the condition. Blood tests may be run to determine if you are malnourished or dehydrated, or have an infection or blood sugar issues. A majority of the diagnostics, however, are tests designed to measure how well your digestive system is functioning or to gauge the condition of your stomach.
Some of the tests involve using cameras or electronic devices to see what is in your stomach. Another possibility is the use of an electronic “pill” that measures how long it takes to move through your digestive system after you swallow it. Your doctor may also order a gastric scintigraphy, which involves scanning your stomach a few hours after eating a small amount of radioactive food to see how much is still left.

6. Dietary Treatment for Gastroparesis
The most important treatment for gastroparesis is dietary. Changes to what you eat, how much and how often are critical in helping to control your symptoms. Avoid foods that are high in fat, as they are difficult to digest. Also avoid fibrous foods that are not cooked until soft. This means eating your vegetables well-cooked instead of raw.
Consuming supplement drinks can help you get the nutrition you are missing from your diet. It can also be helpful to eat less food more frequently. Broths and soups are good choices. Eat a few hours before bed to give your food a chance to digest; otherwise, laying down can result in acid reflux or vomiting.

7. Medications for Gastroparesis
There are not many options for medications that are proven effective for gastroparesis. Many of those available have side effects that make taking them more troublesome than the symptoms you are trying to treat.
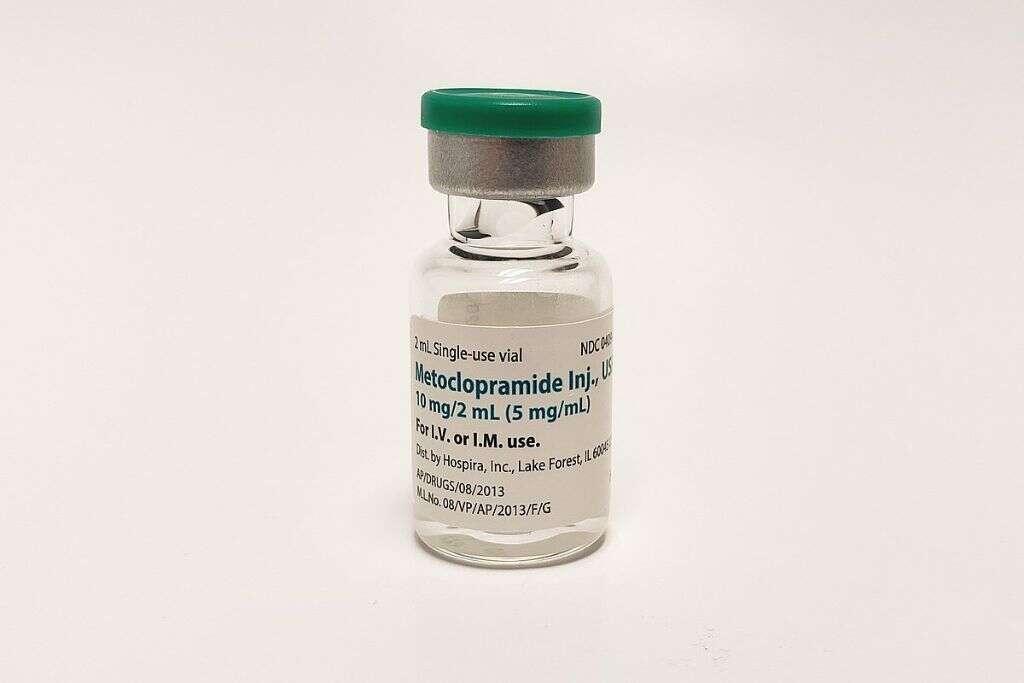
Metoclopramide is a medication that interacts with dopamine receptors and can help stimulate the muscles in the stomach to contract. It has also been shown to reduce nausea. Erythromycin is an antibiotic that is sometimes prescribed to aid in muscle contraction, but its benefits are not long-lasting. A final option, with limited availability, is Cisapride. This medication binds with serotonin receptors and can also help to stimulate the stomach muscles.
8. Surgery for Gastroparesis
Surgery is considered a last resort treatment option. It is rarely used and only for those whose symptoms are severe and don’t respond to other approaches. Surgery may also be suggested if malnutrition is present and cannot be quickly or sufficiently remedied.
Possible medical procedures typically involve placing tubes in the stomach to improve the venting of excess air or to deliver nutritional supplements. On occasion, gastric bypass surgery is done. Complete removal of the stomach is very rarely recommended.

9. Electric Stimulation for Gastroparesis
The delivery of small electrical currents to the stomach can stimulate the muscles to contract more regularly. In this procedure, electrodes are attached inside the lining of the stomach wall. Low-level currents from the electrodes cause the muscles to contract.
Interestingly, this does not improve the stomach’s ability to empty out food. However, it does offer symptomatic relief. Patients who experience nausea and vomiting find that these symptoms become much less problematic following the insertion of such a device.

10. Experimental Treatments for Gastroparesis
A few experimental treatments are being tested to treat gastroparesis. One of these is a class of medications that bind to serotonin receptors, commonly used to treat depression and migraines. They have also been used successfully to treat other conditions that involve reduced muscle use and show promise for those with gastroparesis.
Another treatment being investigated is the use of ghrelin agonists. These medications have the potential to increase how quickly the stomach empties and how fast food moves through the small intestines. Another class of medications is being tested for improving the digestion of fatty foods.