What Is Flesh Eating Bacteria?
Flesh-eating bacteria is the name given to a group of organisms that cause flesh-eating disease, formally called necrotizing fasciitis. This is an infection that spreads rapidly and is cause for serious concern. The disease is rare and treatable, but early care is imperative.
Flesh-eating disease typically occurs in a location where a wound is already infected. The disease leads to tissue necrosis, or death. Necrotizing fasciitis can occur in any location on the body, though the likelihood of contracting the disease anywhere is small.

1. Causes of Flesh-Eating Bacteria Disease
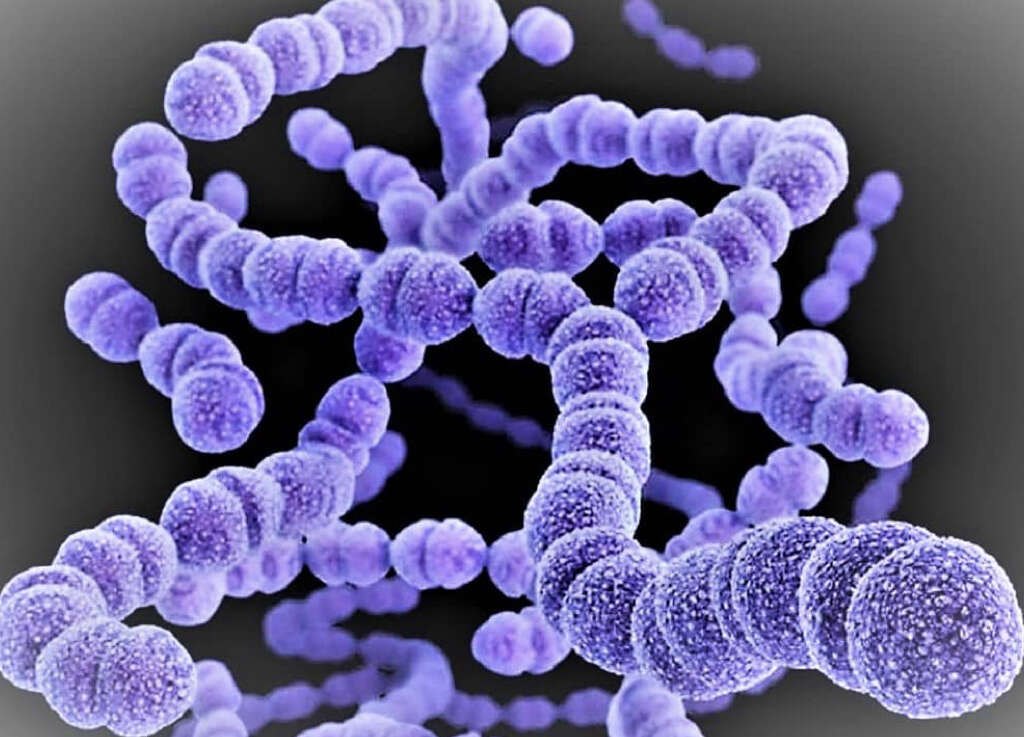
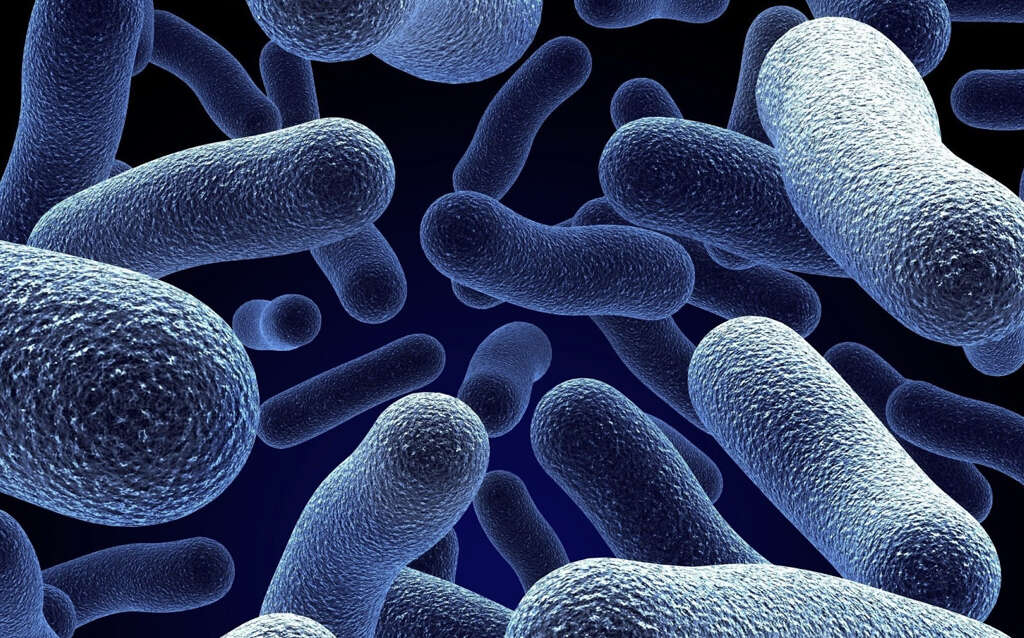
The infection’s primary cause is bacterial, though on occasion a fungus is responsible. Streptococcus and Staphylococcus are the most common bacteria that cause necrotizing fasciitis. Another source, which is rare but increasing, is the Vibrio vulnificus bacterium.
Flesh-eating bacteria disease occurs at a location where another infection is already present. Scientists suspect that this is because non-anaerobic microorganisms damage tissue sufficiently to reduce the levels of oxygen present. This allows the anaerobic bacteria that cause necrotizing fasciitis to flourish.
2. Types of Flesh-Eating Bacteria Disease
The disease is sometimes broken down into three different categories, which are based on the type of organism that causes the infection as well as the clinical findings typical of the specific variety. Type 1 necrotizing fasciitis can be caused by multiple genera of bacteria, Vibrio vulnificus or sometimes a fungus. Type 2 is caused by Streptococcus and Staphylococcus, while type 3 is caused by Clostridium bacteria.
This classification system is infrequently used because the clinical findings in one category can sometimes occur in infections in another. For example, in the type 3 class, the identifying characteristic is a gas that is found in the tissues of the infected person; however, this trait is also seen on occasion in the other two types. For this reason, clinicians typically stick to identifying the disease solely by the bacteria causing it.
3. Introduction of Flesh-Eating Bacteria into the Body
The microorganisms generally enter in areas where the skin is broken, such as cuts, insect bites and puncture wounds. However, the infection can also begin at the site of a trauma where the skin is not broken.
An infection from Vibrio vulnificus can lead to internal flesh-eating bacteria disease. Generally, this occurs when someone with an immune-compromised system eats a contaminated oyster. It can also happen when the individual enters the ocean with an open wound.

4. Symptoms of Flesh-Eating Bacteria Disease
The symptoms for necrotizing fasciitis can be mistaken for a standard infection in the beginning, but they rapidly become increasingly severe. Symptoms can include a wound that worsens instead of healing, pain that extends beyond the site of the injury and is more severe than would be expected, fever, chills and fatigue.
As the disease progresses, symptoms grow more serious. Skin ulcerations, blistering and discolorations are common indicators that the infection is getting worse. Black scabs can also appear as tissue begins to die. Fluid or pus that drains off from the wound rapidly is another symptom. When the infection enters the bloodstream, symptoms of septic shock occur, including rapid breathing, low blood pressure and altered mental states.

5. Complications of Flesh-Eating Bacteria Disease
Unfortunately, it is not uncommon for flesh-eating disease to result in serious complications. Sepsis is one likely outcome, especially since it can occur before a person is aware that they have the disease. Organ failure is another potential complication.
The infection frequently progresses far enough to cause significant damage to the affected area. This can result in, at minimum, scarring. When the infection is severe enough, amputation is sometimes required.

6. Risk Factors for Flesh-Eating Bacteria Disease
Though necrotizing fasciitis is a rare disease, it has to potential to affect people of all ages and both sexes. However, there are people who are more susceptible to getting it. A majority of those who contract flesh-eating bacteria disease have suppressed immune systems.
The types of conditions that increase a person’s vulnerability to the disease include diabetes, cancer, kidney disease and cirrhosis of the liver. The increased risk is likely due to the fact that these individuals have a difficult time fighting off infections in general.

7. Diagnosis of Flesh-Eating Bacteria Disease
Initial diagnosis is typically made through an evaluation of symptoms. The physician also assesses the patient’s medical history for potential risk factors, such as diabetes, as well as means of exposure and routes of infection. Treatment is generally started before further analysis is completed, as delays increase the likelihood of complications, including death.
Sample fluids or tissues are also collected from the infected site. These samples are analyzed to determine the particular bacteria causing the disease, which may alter the course of treatment. Blood and other tests are often also completed to establish and monitor the patient’s overall condition and treatment progress.

8. Treatment of Flesh-Eating Bacteria Disease
Treatment typically begins as soon as possible, prior to final test results. A patient who has been preliminarily diagnosed with necrotizing fasciitis is immediately hospitalized and given intravenous fluids and antibiotics. Many doctors prescribe multiple types of antibiotics concurrently to fight the flesh-eating bacteria as well as the non-anaerobic bacteria.
Surgery is also a first-line-of-defense treatment. It is imperative to remove infected and dead tissue as quickly as possible. Multiple surgeries are usually done throughout the course of treatment. Individuals with flesh-eating disease often require admission to intensive care, where they are treated for complications such as sepsis along with the infection itself.

9. Prognosis for Flesh-Eating Bacteria Disease
Though fewer than 6-7% of people who contract streptococcus infections get necrotizing fasciitis, a third of those who do contract it die, even with treatment. For those who get streptococcal toxic shock syndrome as well as flesh-eating bacteria disease, 60% die from the infection.
Early treatment is the key to a better prognosis; however, significant morbidity, including significant scarring and loss of limb, occurs in many cases. The combined rate for mortality and morbidity is as high as 80%. Without treatment, the prognosis is very poor, and death is a common outcome.

10. Prevention of Flesh-Eating Bacteria Disease
Flesh-eating bacteria require an initial infection before they are able to thrive. Therefore, the best way to prevent the disease is to prevent primary infections from occurring. Cleaning cuts and abrasions, covering open wounds until they heal and going to the doctor for deep puncture wounds are measures that significantly reduce the chances for flesh-eating bacteria disease.
Fungal infections need to also be treated. Anyone with an open wound should refrain from using hot tubs or swimming in pools, lakes, rivers or the ocean. There are no vaccinations available to prevent necrotizing fasciitis.