What Is Dermatomyositis?
Not many people have heard of dermatomyositis as it is a very rare condition affecting the connective tissues of the body, making it similar to other connective tissue diseases such as lupus erythematosus and systemic sclerosis. The condition affects both the muscles and the outer layer of the skin.
For individuals living with this inflammatory disease, it can be difficult to get the facts since there is still much information that is not known about dermatomyositis. Designating funds and getting public support for gathering research on this condition is essential for helping people find relief. While there are many gaps in knowledge, answers to these questions about the illness help provide some guidance.

1. How Is Dermatomyositis Related to Myositis?
Dermatomyositis is actually a subcategory of myositis. While the word myositis is often used to describe all kinds of muscle swelling, the condition of myositis refers specifically to any type of disease that involves chronic muscle inflammation. Many of the ailments that fall under this category are also autoimmune conditions.
The five main types of myositis include dermatomyositis, polymyositis, necrotizing myopathy, sporadic inclusion body myositis, and juvenile myositis. The symptoms for all these conditions vary, and they primarily affect different age groups and genders.

2. What Are the Symptoms of Dermatomyositis?
The indications of dermatomyositis can differ from person to person, but the main symptoms people often exhibit include general muscle weakness and soreness accompanied by skin rashes. People may also experience fatigue, difficulty swallowing, and shortness of breath. Individuals who only have a skin rash but no muscle weakness may receive a diagnosis of amyopathic dermatomyositis.
Often, the rash is the first sign of dermatomyositis, which can cause rough patches on the skin, swelling around the fingernails, purple-colored eyelids, and a dark rash on the face, neck, shoulders, chest, back, and knuckles. Later on, muscle weakness starts to settle in, starting with lower body parts, such as the back or hips, and working its way up the body. Pain may accompany the weakness as well.

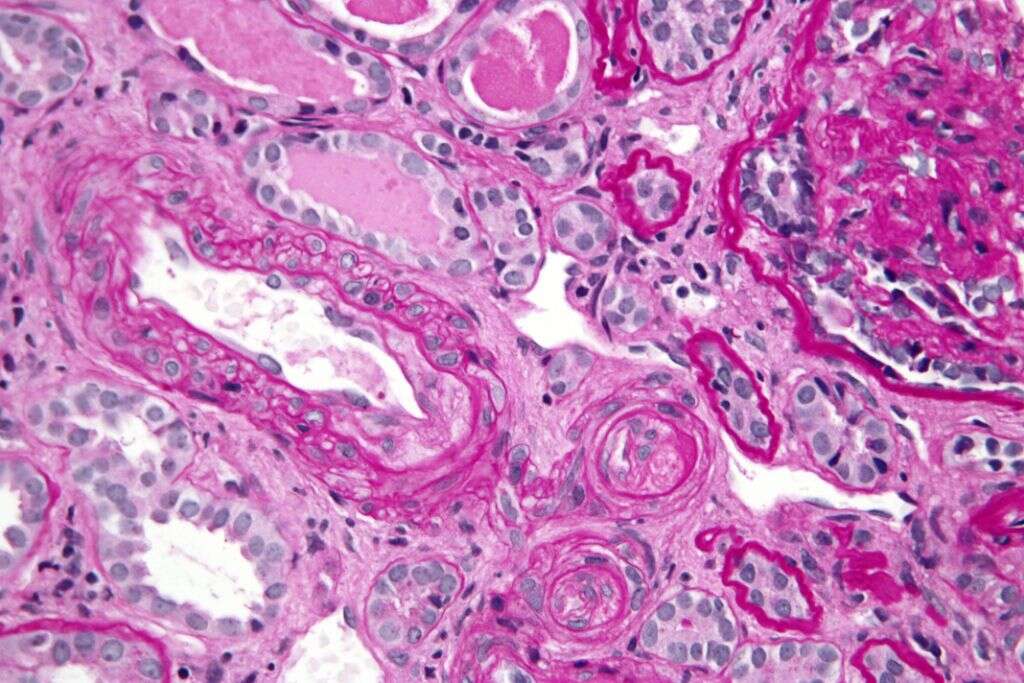
3. What Causes Dermatomyositis?
While there are many known causes of myositis, including infection, drug use, and injury, there is little known about why some people develop dermatomyositis. It may be caused by microangiopathy, which is a disease affecting small blood vessels. There seems to be a strong genetic component, especially for younger patients who develop dermatomyositis.
Other suspected causes of dermatomyositis include cancer in older adults, an autoimmune reaction, an effect of certain drugs, or the result of specific toxins. It is thought a combination of environmental and biological factors are to blame.
4. Who Is Most Often Affected by Dermatomyositis?
Potentially, anyone can be affected by dermatomyositis. However, there are certain populations that may be more susceptible than others. It is most common among children between the ages of 5 and 15 and adults between 40 and 60. Also, women are more likely to get dermatomyositis than men.
People with certain autoimmune disorders may be at more risk since it is believed the condition can be caused by a defect in the immune system’s response. Essentially, the immune system is attacking body tissues. Additionally, people with certain types of cancer, including those in the abdomen or lungs, are more susceptible.
5. Are Children Affected the Same as Adults?
When a child develops dermatomyositis, the disease is often referred to as juvenile dermatomyositis. Many of the symptoms are the same among adults and children, including muscle inflammation and skin rash. The onset for children is often between the age of 5 and 10.
While both children and adults may experience calcium deposits under the skin, this symptom is more common in children with the condition. Some children may recover completely from dermatomyositis, while others will have symptoms that continue into adulthood. In general, children are more likely to eventually experience cessation of symptoms than adults with dermatomyositis.

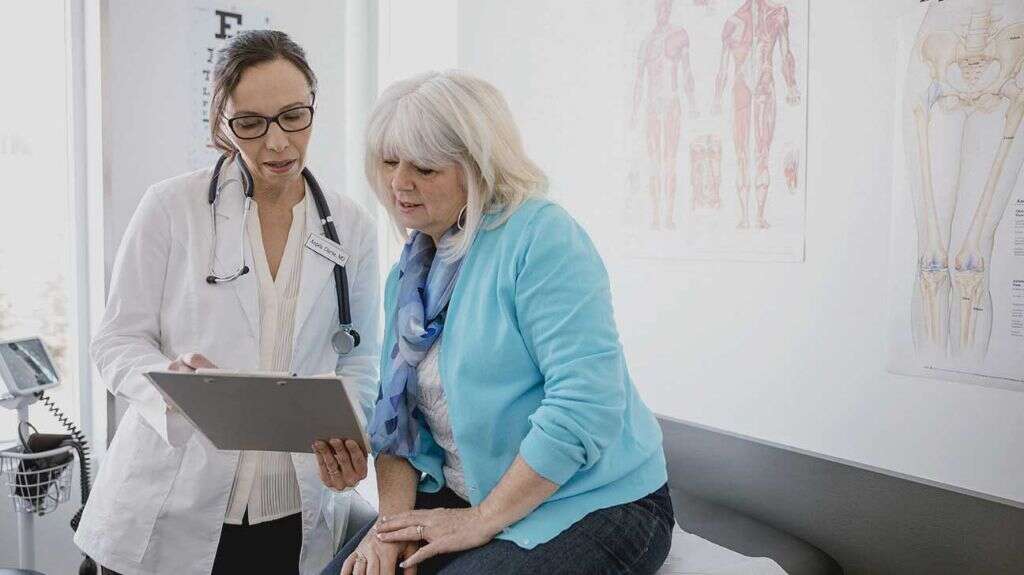
6. How Is Dermatomyositis Diagnosed?
To diagnose dermatomyositis, the doctor examines the patient’s symptoms, looks for signs of rash, and asks about any muscle weakness or pain. The physician may also perform a swallowing study if the patient complains of any difficulties swallowing.
Several other tests can aid the doctor in making a diagnosis. These may include cancer screening, a blood test for autoimmune disorders, ECG, MRI, chest x-ray, and a lung function test. There are also tests for detecting certain myosotis-specific autoantibodies.

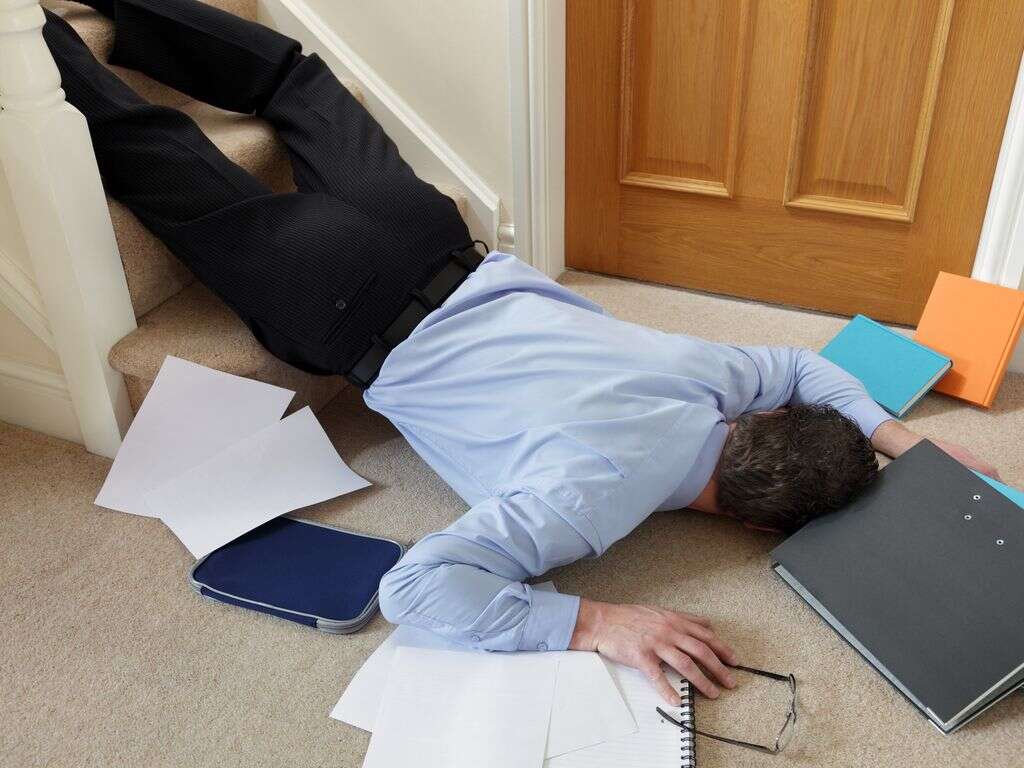
7. Is Dermatomyositis Dangerous?
While dermatomyositis is a chronic condition and may not be dangerous for all patients, several potential complications can harm or even cause death for the patient. For example, muscle weakness can lead to various falls and accidents.
Sores can turn into ulcers that can become infected. Cancer and lung disease that sometimes contribute to the condition can be fatal. Additionally, pain or difficulty swallowing may lead to malnutrition and weight loss.
8. Can Dermatomyositis Be Cured?
Currently, there is no known cure for dermatomyositis. While some people, especially children, may see a full remission, others go on to live with the disease for the rest of their lives. The condition resolves itself for about 20% of patients.
Some research suggests that addressing the illness early on can improve the overall prognosis. Since there is no medical cure available that can completely get rid of dermatomyositis, most treatments have the goal of easing symptoms and making life as enjoyable as possible for the patient.
9. What Are the Treatment Options for Dermatomyositis?
There are several regimens to address symptoms of dermatomyositis. Often, the process starts with a heavy dose of medicine initially that is followed by smaller doses until muscle strength returns. However, many people may need to continue with the prescribed medicine for the rest of their lives if the condition does not go away on its own.
Corticosteroid medicines are the primary treatment for people with dermatomyositis. Immune suppressants, such as azathioprine, mycophenolate, and methotrexate, are also used. If these treatments are not successful, the doctor may prescribe intravenous gamma globulin or biologic drugs. After strength returns, the patient may need to continue with prednisone.

10. What Research Is Being Done to Better Understand Dermatomyositis?
Since there is still so much unknown about dermatomyositis, research is necessary to comprehend what causes the condition and find out any other treatment options doctors should explore. Both ClinicalTrials.gov and the Autoimmune Registry are known organizations that are currently conducting trials and gathering research on the condition.
There also several groups that are dedicated to funding research toward this disease, including Myositis UK, The Myositis Association, Myositis Support and Understanding, and Cure JM Foundation. The American Autoimmune Related Diseases Association also provides support toward this cause.












