What Is Apnea?
Apnea occurs when there is a temporary cessation of breathing. When there is apnea, the muscles of inhalation are not moving, causing the lung volume to remain unchanged. Depending on the patency of the airways, there may or may not be any flow of gas between the environment and lungs.
Apnea can be drug induced, mechanically induced, due to trauma, voluntarily achieved (via breath-holding), or as a complication because of a neurological disease. When it lasts for more than one minute, apnea can result in severe lack of oxygen in the body. Unless ventilation is restored, in as little as three minutes, permanent brain damage can occur. Several more minutes and death may occur. Sleep apnea can be generally categorized into obstructive sleep apnea (OSA), central sleep apnea, and mixed apnea.
1. Mechanism
Besides occurring voluntarily, or by drug use, mechanical reasons (choking or strangulation), trauma, heightened emotion, breath holding spells (emotional stress, frustration, other psychological issues), and neurological disease, it can also occur during sleep. This is known as sleep apnea. For patients who suffer from sleep apnea, the episodes of apnea can occur more than a hundred times every hour during sleep.
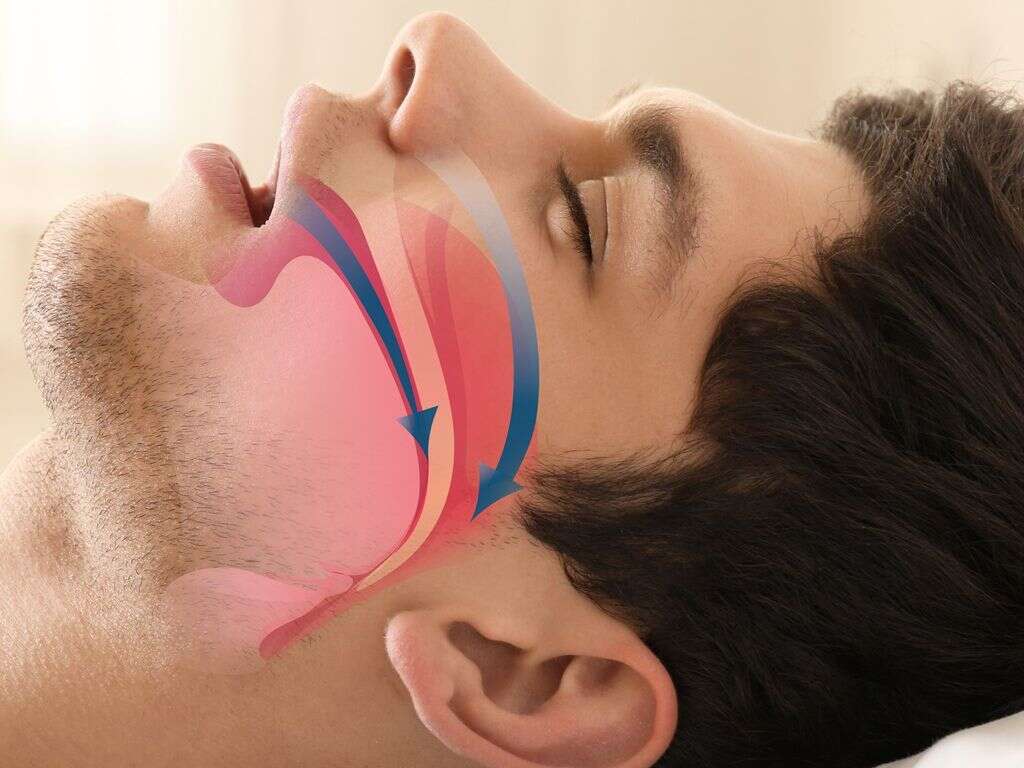
In obstructive sleep apnea, the muscles in the back of the throat relax causing the narrowing of the airway. These muscles are responsible to support the uvula, soft palate, tongue, and tonsils. As it relaxes, the tissues are not supported. This can result in gasping, snorting, or choking. In central sleep apnea, it occurs when the brain is unable or fails to send signals to the breathing muscles.

2. Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a condition where there is decreased airflow despite breathing. It is the commonest sleep-disordered breathing (SDB) characterized by recurrent collapse of upper airways during sleep. These episodes cause the patient to wake up repeatedly resulting in poor sleep quality and fatigue in the daytime.
Although common, it is underrecognized by most primary care practitioners with an estimated of 80% of Americans being undiagnosed. Episodes of apnea can occur 1 to 2 times per minute resulting in hundreds of episodes every night. In severe OSA, there can be decreased oxygen saturation and wide swings in heart rate. In sleep apnea, the cardinal symptoms are snoring, significant other reporting of apnea episodes, and sleepiness.
3. Causes of Obstructive Sleep Apnea
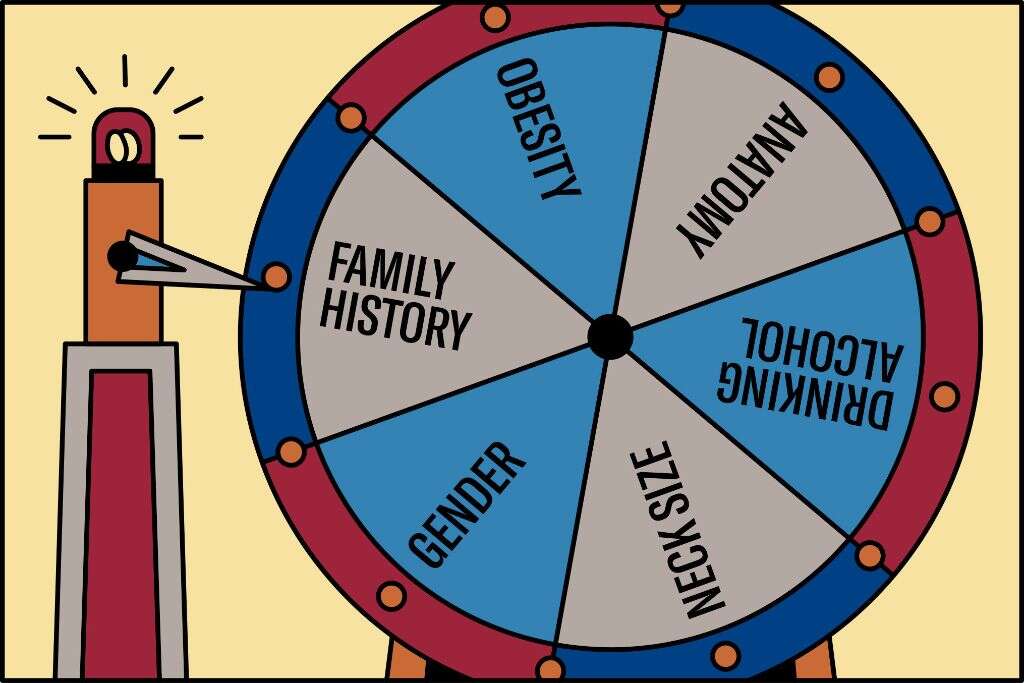
Causes of OSA can be divided into genetic, structural, and nonstructural factors. For structural factors, it involves the anatomy of the face and head that may increase the likelihood for OSA.
For example, when there is posterior facial compression, facial elongation, mandibular hypoplasia (small jaw), retrognathia (abnormal positioning of the maxilla or mandible) or micrognathia (undersized jaw), adenotonsillar hypertrophy (increased size of tonsils), high arched palate, deviation of the nasal septum, polyps, tumors, and more. Studies have shown that these abnormalities are a significant cause of OSA for nonobese patients. Nonstructural risk factors include obesity, alcohol use, sedative use, smoking, supine sleep position, hypothyroidism, stroke, neurological issues, and more.

4. Epidemiology of Obstructive Sleep Apnea
In today’s modern society, OSA is increasingly prevalent regardless of age. Various studies have estimated the prevalence of OSA to range from 2% to 9% for women and 4% to 24% for men. In children, the prevalence is less certain but the numbers are increasing due to higher rates of obesity.
Globally, the prevalence of OSA has only been studied in men and varies between regions. Aging is a major risk factor for OSA with prevalence increasing 2 to 3 times in individuals above the age of 65 years old. Males are also more likely to have OSA compared to females (at a ratio of 2 to 3:1). This has been attributed to the androgenic patterns of fat distribution in the trunk and neck area. African Americans are also predisposed to OSA compared to Caucasians. Asians also have a higher risk due to their craniofacial structure (more crowded upper airway, retrognathia, and shorter and more acute cranial base).
5. Signs and Symptoms of Obstructive Sleep Apnea
OSA symptoms at night may include loud snoring (to the point that it bothers others), gasping , snorting, or choking that causes arousal, insomnia, nocturia, restless sleep, witnessed apneas (by sleeping partner), and restless sleep.
During the day, patients may experience a headache, sore throat, nonrestorative sleep (tired as soon as waking up), memory impairment, difficulty with concentration, personality changes, irritability, depression, hypertension, gastroesophageal reflux, decreased libido, sexual dysfunction, morning confusion, decreased reflexes, and more. In children with OSA, there may be reduced growth rate due to intense effort required for breathing causing calories to be burned at high rates and an obstructed nose and throat causing decreased taste and appetite.

6. Diagnosis
Patients with excessive daytime sleepiness should undergo a sleep study such as a polysomnography. Routine laboratory tests have little to no purpose in OSA unless there is a specific indication. In patients suspected with hypothyroidism, a thyrotropin test can be performed especially among elderly patients.
One study found that cysteine levels may be a potential biomarker for OSA as it was found to be higher in OSA patients and reduced once effective OSA treatment was provided. A randomized controlled study reported that home oximetry may be a method to help diagnose OSA as it is easier to obtain compared to polysomnography. This test is a non-invasive method that monitors the oxygenation in the blood. However, as it does not measure apneic events, it does not produce an apnea-hypopnea index (AHI).

7. Treatment of Obstructive Sleep Apnea
Treatment of OSA includes avoiding the use of tobacco and alcohol. Medications that help relax the central nervous system such as muscle relaxants and sedatives should also be avoided. Weight loss is generally beneficial especially for those who are overweight.
Mandibular advancement devices and continuous positive airway pressure are generally effective for patients with OSA. Regular exercise even if there is no weight loss has been found to improve sleep apnea. Surgical treatments to improve the anatomy of the airway can also be beneficial. However, it should not be a frontline treatment. Some of the surgeries that can be performed are tonsillectomy, adenoidectomy, septoplasty, turbinectomy, and more. Patients who are morbidly obese will benefit from bariatric surgery to help weight loss. Evidence to support medication use such as paroxetine, fluoxetine, tryptophan, and acetazolamide is insufficient.
8. Central Sleep Apnea
Central sleep apnea (CSA) is a disorder where there is reduced or absent effort to breathe for about 10 to 30 seconds. This can occur in cycles or intermittently and generally causes a decreased oxygen saturation in the blood. It is believed to be due to an instability in the feedback mechanisms in the body.
It can be caused by an underlying medical condition, use of narcotics, ascent to high altitude, and more. Primary central sleep apnea is rare and not entirely understood. Like OSA, patients with CSA present with excessive daytime sleepiness, snoring, nonrestorative sleep, nighttime awakenings, and more. Insomnia is also more prevalent among CSA patients compared to OSA. Depending on the underlying cause of CSA, the patients may experience symptoms from that condition as well.

9. Causes and Statistics
CSA can occur due to ventilatory instability and depression of the respiratory centers in the brainstem or chemoreceptors. CSA can be seen in Cheyne Stokes breathing (due to renal failure, stroke, heart failure) or has an underlying disorder (such as diabetes mellitus, hypothyroidism, Parkinson’s disease, muscular dystrophy, myasthenia gravis), at high altitudes (some may experience it at 5,000 meters or more while almost all develop it at 7,600 meters), and use of central nervous system depressants or opiates.
CSA is uncommon and is estimated to have a prevalence of less than 1% in the general population. It does not have a racial predilection. Males are more likely to be affected compared to females. It also tends to affect middle-aged or elderly individuals and is found to have a higher prevalence among those above the age of 60 years old.
10. Diagnosis, Treatment, and Prognosis
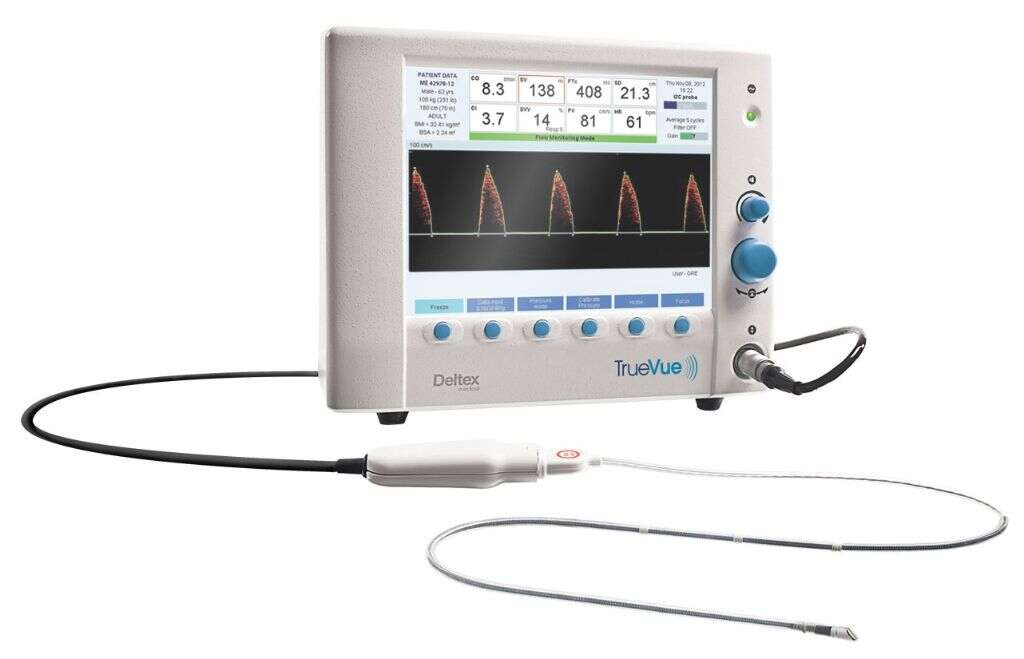
Diagnosis generally requires a sleep study performed at a sleep lab. Laboratory studies are generally beneficial to help rule out other causes or to determine underlying causes. Imaging studies are needed, such as a computed tomography (CT) scan and magnetic resonance imaging (MRI), to determine underlying causes such as an Arnold-Chiari malformation, stroke, tumor, and more.
Most diagnoses can be made based on polysomnography. An esophageal pressure monitoring using a balloon catheter, echocardiography, and home monitoring devices can also be used. There are no clear guidelines for the treatment of CSA. A pacemaker-like device known as the remede system can help moderate to severe CSA. A bilevel positive airway pressure (BiPAP) and continuous positive airway pressure (CPAP) can also be used.