What Is Acute Cholecystitis?
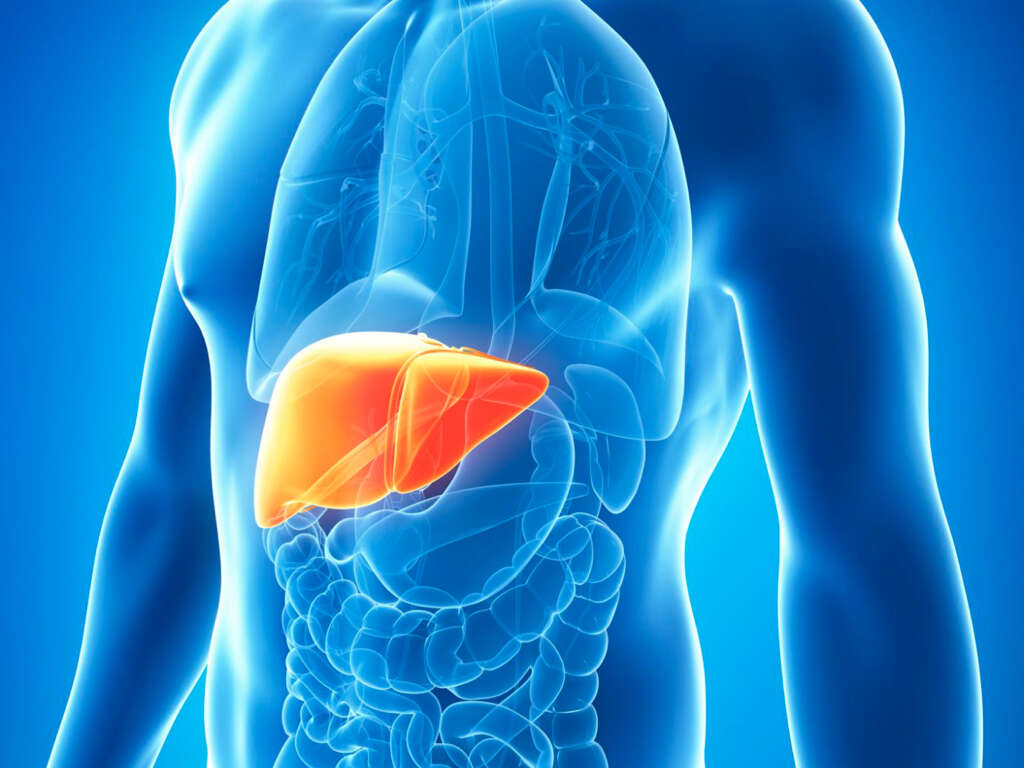
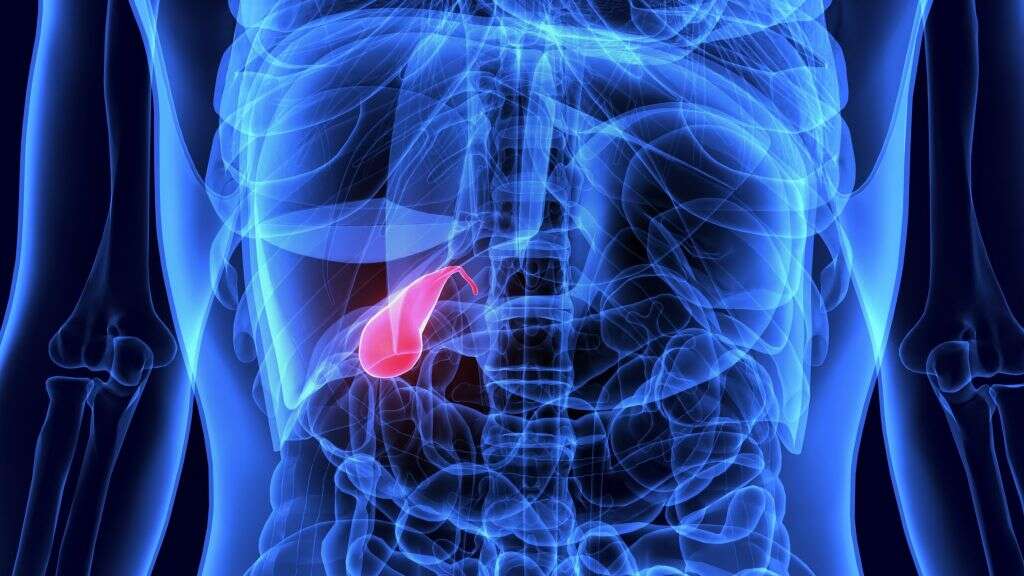
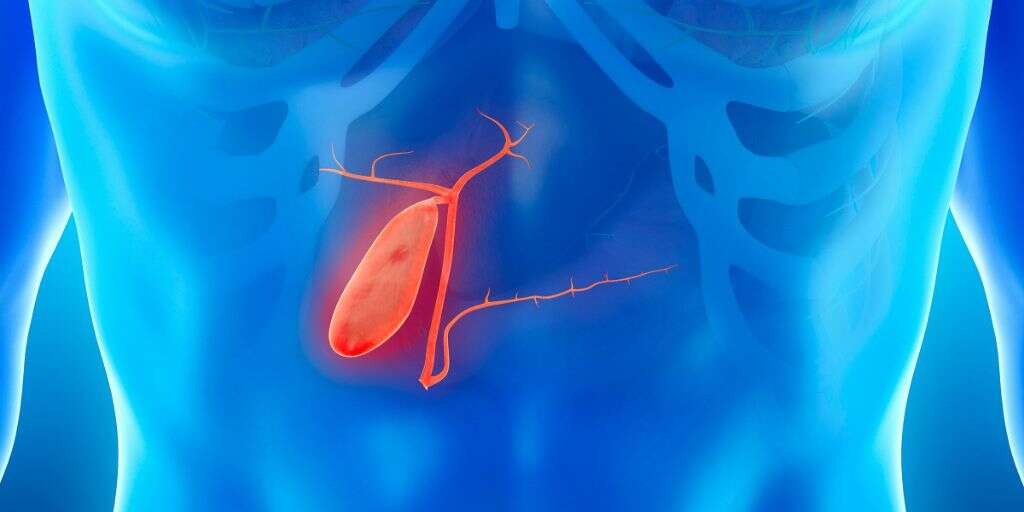
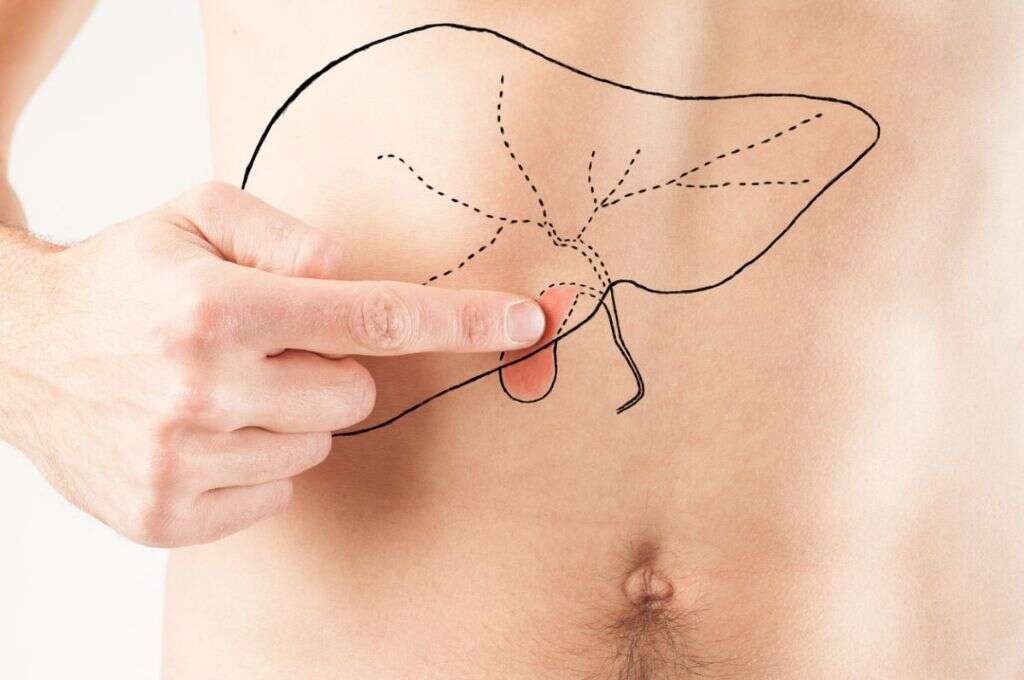
The gallbladder is an organ that’s responsible for holding and releasing digestive fluid called bile into the small intestine. It’s a small organ that’s shaped like a pear and located beneath your liver on the right side of your abdomen.
When the gallbladder works properly, you hardly even know it’s there. But when the tube that leads out of the gallbladder becomes clogged, it can lead to a painful condition known as acute cholecystitis.
1. What Is Acute Cholecystitis?
Acute cholecystitis is inflammation in the gallbladder that develops over a period of several hours. It is also commonly referred to as a gallbladder attack. If the tube that leads out of your gallbladder is blocked by gallstones, cholecystitis is often the result. As bile continues to build up in the gallbladder, it can lead to significant pain and even death.
In addition to gallstones, acute cholecystitis can be caused by anything else that blocks or damages the bile duct. Examples of other common causes for acute cholecystitis include tumors, infections and certain serious illnesses.
2. What Are the Symptoms of Acute Cholecystitis?
Symptoms of acute cholecystitis often include severe pain that is usually felt in the upper-right part of the abdomen. Some people may feel shortness of breath or pain that radiates into the right shoulder. Other possible symptoms include fever, nausea, sweating, loss of appetite, vomiting and jaundice (yellowing of the whites of the eyes and the skin).
If you experience jaundice or fever in combination with severe abdominal pain, it’s important to seek medical treatment immediately. These are signs of an infection and could potentially lead to serious medical complications or even death if left untreated.

3. Can Acute Cholecystitis Lead to Chronic Cholecystitis?
Chronic cholecystitis is inflammation of the gallbladder that persists for long periods of time and recurs frequently. Chronic inflammation of the gallbladder is almost always due to gallstones. Those who have chronic cholecystitis may have an increased risk of gallbladder cancer.
If you experience repeated episodes of acute cholecystitis, you’re more likely to be diagnosed with chronic cholecystitis. It’s possible for the gallbladder to become damaged by repeat gallbladder attacks over time, which is why treatment is so important.
4. What Are the Risk Factors for Acute Cholecystitis?
As with most other diseases and illnesses, there are certain risk factors that can make you more likely to get acute cholecystitis. While gallstones are the main risk factor associated with this condition, there are others as well.
If you are middle-aged or older, have a family history of cholecystitis or are overweight, you may have an increased chance of developing acute cholecystitis. Women and people of Native American, European or Hispanic heritage are also at increased risk. Though less common, cholecystitis without gallstones may occur after intravenous feeding, multiple organ failure, cardiovascular disease and serious burns.
5. Is Gallbladder Inflammation More Prevalent During Pregnancy?
A person’s risk of developing gallstones increases during pregnancy. This also means that the risk of gallbladder inflammation goes up when an individual is pregnant. Surgery is often recommended to remove the gallbladder if cholecystitis occurs during the course of pregnancy. This is usually done laparoscopically to avoid complications.
Some doctors may not be comfortable removing the gallbladder while a woman is pregnant. They may decide to treat the condition with antibiotics, pain relief medications and fluid replacement until after the baby is born. However, the risk of complications to both the mother and baby may increase if surgery is delayed.

6. What Complications Can Result From Acute Cholecystitis?
Since pain from cholecystitis is often extremely severe, those who experience it usually opt to receive treatment right away. However, if cholecystitis is not treated, a variety of complications can result. Some may be life-threatening.
Possible complications of untreated gallbladder inflammation include gallbladder perforation and gangrenous cholecystitis. The former condition is characterized by a gallbladder rupture which leads to leaking bile. This condition can cause an infection within the abdomen. Gangrenous cholecystitis occurs when tissue in the gallbladder dies and becomes susceptible to infection. It isn’t unusual for gangrenous cholecystitis to lead to sepsis, which is a life-threatening condition in which the entire body responds to an infection in the blood.
7. How Is Acute Cholecystitis Diagnosed?
A doctor may take several steps to diagnose acute cholecystitis. A diagnosis may include a physical examination, blood tests, a computed tomography scan or other imaging tests.
If a doctor thinks you have gallbladder inflammation, he or she may order additional tests, including abdominal ultrasounds, an MRI, cholangiography, X-rays or hepatobiliary scintigraphy. These are all different types of tests that can confirm the diagnosis of gallbladder inflammation. If the condition is confirmed, your doctor may recommend you to a hospital for prompt treatment.

8. What Are the Treatment Options?
The type of treatment your doctor recommends depends on the severity of your condition as well as its underlying cause. Usually, initial treatments involve pain relief measures, antibiotics if an infection is present, and intravenous fluids to prevent or treat dehydration. If the condition is mild, treatment may not require a hospital stay.
In severe cases of cholecystitis, hospitalization and surgery may be required. Surgical removal of the gallbladder can be done in two ways: laparoscopic cholecystectomy, in which the gallbladder is removed through a small abdominal incision, or open cholecystectomy, where the gallbladder is removed through a large incision made in the abdomen. In cases where surgery is not an option because the risks are too great, a doctor may drain the gallbladder through endoscopic ultrasound-guided transmural cholecystostomy.

9. What Is Post-Cholecystectomy Syndrome?
Post-cholecystectomy syndrome affects approximately one in 10 people after gallbladder removal. The causes of this condition are not completely understood, but it is thought to occur when the sphincter of Oddi muscle spasms or becomes scarred after surgery. Post-cholecystectomy syndrome is associated with a variety of symptoms, including severe pain in the abdomen, vomiting and nausea. A blood test, colonoscopy, ultrasonography or magnetic resonance cholangiopancreatography may all help diagnose the issue and rule out other structural GI problems.
Endoscopic treatments for post-cholecystectomy syndrome may help relieve pain and restore bile flow. Dietary restrictions may also be recommended to help reduce the secretion of digestive enzymes and give the bowels a rest.

10. How Can You Prevent Gallbladder Inflammation?
It may not always be possible to prevent the development of gallbladder infection. However, there are some steps you can take to reduce your risk. It’s particularly important to focus on reducing your chances of developing gallstones, which are a primary cause of gallbladder inflammation.
Eating a healthy diet is the best way to avoid gallstones. Avoid taking in too much fat and eat plenty of fruits, vegetables, whole grains and beans. Regular exercise and preventative medication can also help lower the risk of gallstones in individuals who have a family history of the condition.