What Is a Frozen Shoulder?
A frozen shoulder, or adhesive capsulitis, refers to a stiff and painful shoulder. Per the American Shoulder and Elbow Surgeons, a frozen shoulder can be defined as “a condition of uncertain etiology characterized by significant restriction of both active and passive shoulder motion that occurs in the absence of a known intrinsic shoulder disorder.” Meanwhile, the American Academy of Orthopedic Surgeons define it as “a condition of varying severity characterized by gradual development of global limitation of active and passive shoulder motion where radiographic findings other than osteopenia are absent.”
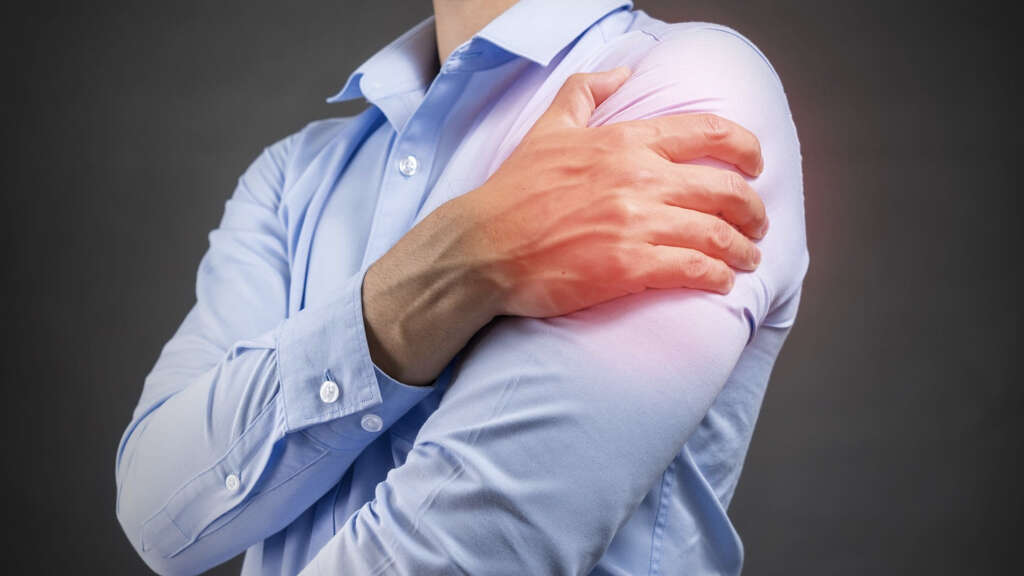
This means that the shoulder capsule is affected. This includes the connective tissue that surrounds the shoulder or glenohumeral joint causing it to become stiff and inflamed. This condition restricts motion and lead to chronic pain. Despite being unclear regarding the cause of frozen shoulder, some believe that it may be caused by trauma or injury to the area while others think it may have an autoimmune component.

1. Epidemiology
Frozen shoulder is observed to most commonly affect patients between the ages of 40 to 60 years old. Although the exact incidence is unclear, it is thought to occur in approximately 2% to 5% of the general population (at some point in life). While women tend to be affected more commonly compared to men, there does not seem to be any predilection for race. Generally, the involvement of both shoulders is rarely concurrently and it tends to occur sequentially. One of the most important risk factors for frozen shoulder is diabetes mellitus. A meta-analysis found that diabetic patients are 5 times more likely to develop this condition compared to their nondiabetic peers. It is estimated that there is a 13.4% overall mean prevalence of frozen shoulder among diabetics and a 30% mean prevalence of diabetes among patients with frozen shoulder.

2. Etiology
Despite not having a precise cause for frozen shoulder, several reported etiologic agents include surgery, diabetes, trauma, inflammatory disease, various shoulder maladies, and regional conditions. An autoimmune theory has also been proposed as patients with frozen shoulder have been found to have higher levels of C-reactive protein and HLA-B27 histocompatibility antigen.
Another expert proposed muscular inactivity as a major cause. Frozen shoulder has also been associated with Parkinson’s disease, hypothyroidism, hyperthyroidism, cervical spine disease, and ischemic heart disease. It has also been noted that the incidence of frozen shoulder is 5 to 9 times higher among neurosurgery patients who have had their shoulders immobilized for varying durations compared to the general population.
3. Stages of Frozen Shoulder
Patients with primary frozen shoulder may have no significant findings in their patient history, physical examination, or radiographic tests. Their condition can be divided into pain, stiffness, and thawing. The stages of frozen shoulder begin at stage 1 where there can be a gradual onset of pain in the shoulder lasting from weeks to months. This can go on for as long as 9 months.
Stage 2 is known as the frozen or stiffening stage where there is progressive loss of range of movement lasting from 4 to 20 months. Most patients lose the ability to abduct, internal rotate, and external rotate during this phase. The final stage or stage 3 is known as the thawing phase that can last from 5 to 26 months. During this phase, there is gradual motion improvement.

4. Patient History
Some of the important points to elicit from the patient would include the onset of symptoms, history of surgery, possible injury or trauma, duration of symptoms, and existing medical conditions (such as diabetes, thyroid disease, stroke). Those with a history of cervical (neck) pain should be evaluated for cervical disc disease or cervical spondylosis.
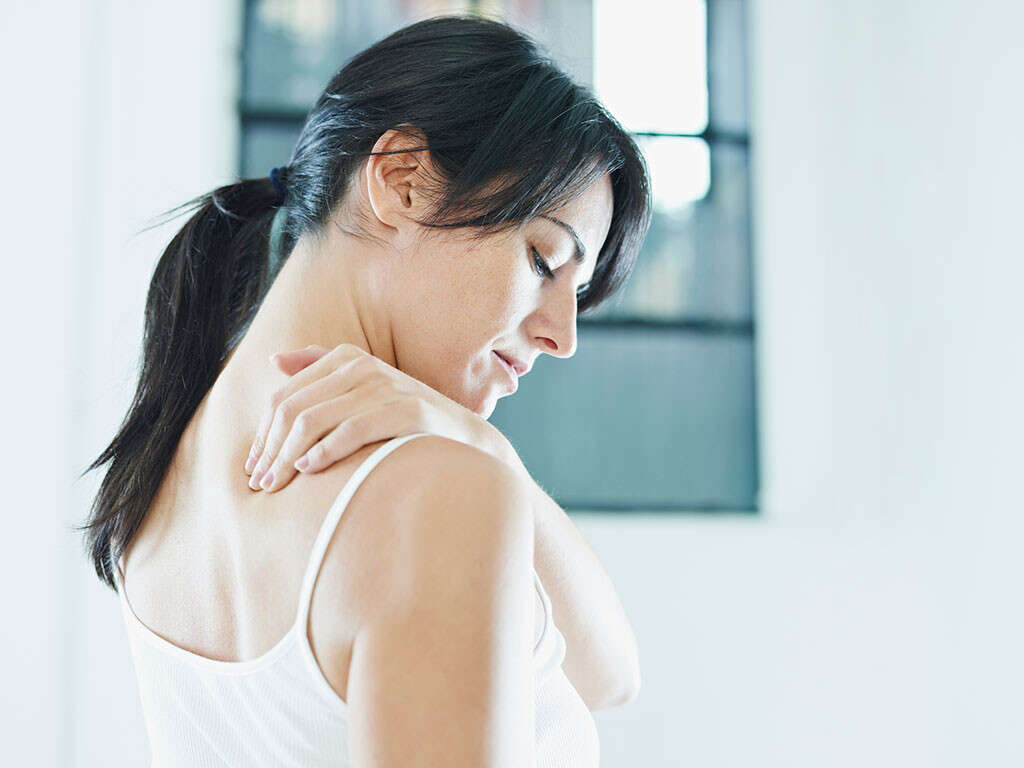
Patients often present with the main complaint of a stiff and painful shoulder. Due to the pain and stiffness, there is also loss of range of motion. Patients with frozen shoulder tend to have constant pain that is worse at night or in cold weather. Movements of the shoulder such as bumps can also lead to cramping and pain.

5. Diagnosis
Since frozen shoulder is mostly a clinical diagnosis, laboratory studies are rarely required. However, if a predisposing condition is suspected to contribute to frozen shoulder, some tests may be beneficial. This includes a complete blood count (CBC), C-reactive protein, erythrocyte sedimentation rate, hemoglobin A1c, blood glucose, free thyroxine, thyroid stimulating hormone, and more.
Imaging studies are not generally indicated. However, routine radiographs can help rule out any pathological process. The use of ultrasonography is controversial but has been shown to be able to measure the thickness of the acromiohumeral ligament, presence of fibrovascular inflammatory tissue, and increased vascularity in the rotator interval. Arthrography can also be helpful. Magnetic resonance imaging (MRI) can help rule out other pathology if the patient does not improve after 6 weeks.

6. Treatment Approach and Medications
In patients with frozen shoulder syndrome, the aims of treatment are to relieve pain and restore function and movement to the shoulder. Since it is self-limiting, the prognosis tends to be similar regardless of the treatment used. The first line of treatment for frozen shoulder would be home exercise and physiotherapy.
These treatments can be combined with glenohumeral joint corticosteroid injection and anti-inflammatory medications. Since more than 90% of patients respond to conservative treatment options, most are treated nonoperatively. Surgery has not been found to improve outcomes. Some of the medications that can be helpful include nonsteroidal anti-inflammatory drugs, oral glucocorticoids, and corticosteroid injections.

7. Surgical Therapy
Surgery is reserved for patients who do not experience any improvement in symptoms despite conservative management. Surgical therapy should be deferred as long as possible. Patients with frozen shoulder who fail to improve despite nonsurgical therapy and medication are known as having recalcitrant or refractory frozen shoulder. These patients demonstrate minimal improvement over 3 months despite aggressive nonoperative measures such as physical therapy and medications; however, it should be noted that it can take much longer than 3 months to move through the stages of a frozen shoulder.
Aggressive nonoperative measures may also be aggravating to the area depending on the stage of frozen shoulder (which can be difficult to identify) thus lengthening the time it takes to recover. In these cases, distention arthrography, manipulation, and open surgical release may be required. Complications that can occur from these therapies include rotator cuff tears, humeral shaft fractures, and transient brachial plexus injuries. After surgery, physical therapy may be required. As stated above, surgery has not been found to improve outcomes.

8. Complications and Prognosis
The main complication reported by patients is the residual stiffness and pain despite healing. There are several reports stating most patients may continue to experience stiffness and/or pain for up to 3 years with conservative treatment. The prognosis for frozen shoulder is good as it is a self-limiting condition that can be managed using physical therapy and usually resolves within 1 to 3 years.
In patients with diabetes, there has been no difference in disability and pain reported compared to nondiabetics. Long-term disability has been reported in as many as 15% of patients, persistent symptoms in 40%, and permanent functional loss in 7% to 15%.

9. Investigational Therapy
An injection treatment known as collagenase clostridium histolyticum (CCH) is approved by the United States Food and Drug Administration for adult patients with Dupuytren contracture. This has been used as a trial in patients with frozen shoulder and has been reported to be well-tolerated and effective compared to exercise. However, more studies will be necessary.
Extracorporeal shockwave therapy (ESWT) has also shown promise for the treatment of frozen shoulder. It has been found to be favorable compared to oral steroids as short-term treatment in a randomized controlled trial. During the 4th week of treatment, the ESWT group had significant treatment compared to those taking steroids. By the 6th week, the improvement in activities of daily living was significantly better than the steroid group. Researchers believe that ESWT may be a safer alternative compared to steroid injections or surgery.

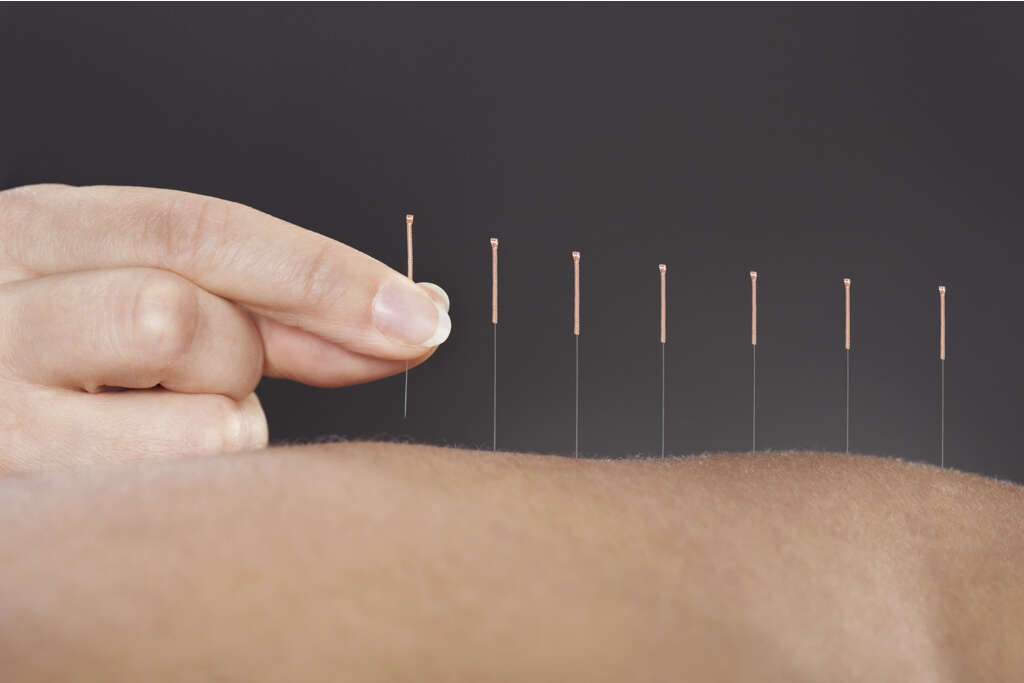
10. Acupuncture
Acupuncture is an effective alternative treatment option for those with frozen shoulder. Acupuncture is a treatment that is about 5,000 years old. It is still being used to cure many diseases, specifically for chronic joint pain. It is a method where very thin needles are used to pierce certain spots of the body for pain relief or for the treatment of a specific problem. The needles are disposable and made from stainless steel.
The World Health Organization (WHO), American Medical Association (AMA), and National Center for Complementary and Integrative Health (NCCIH) have declared that acupuncture can be effective for the treatment of various diseases. Several studies have found that frozen shoulder would be more effectively treated with a combination of shoulder exercises and acupuncture.