What Are Skin Infections?
Your skin is your body’s largest organ. It serves to protect internal organs from the environment and is an extremely effective barrier against germs and many other potentially harmful substances. However, it is not impenetrable.
When the skin is broken, or an open wound or puncture breaks the barrier, germs can get inside the skin’s layers. While your body can fight them off in many cases, they will sometimes lead to an infection. Skin infections range in severity from mild to potentially life-threatening, so they should be taken seriously.

1. What Causes Skin Infections?
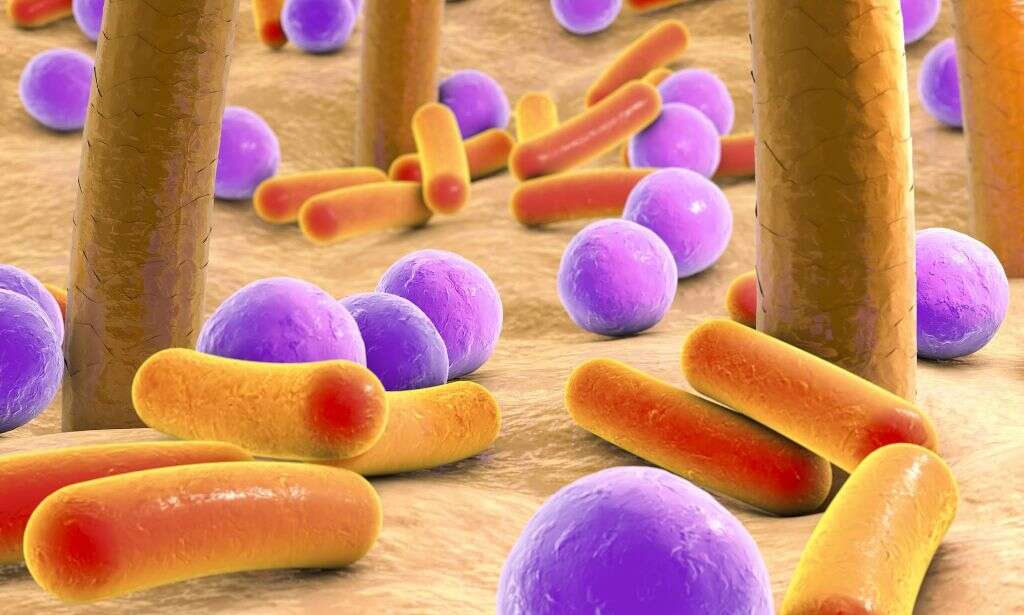
Several things can cause skin infections. Most skin infections are caused by microbes that are present in our skin, soil, or water. Others are caused by pathogens that linger in medical settings. Direct physical contact with an infected individual can also cause an infection.
Bacteria and fungi are the most common pathogens that cause infection. When they manage to enter the skin through a cut or open wound, these germs multiply and infect the surrounding tissue.

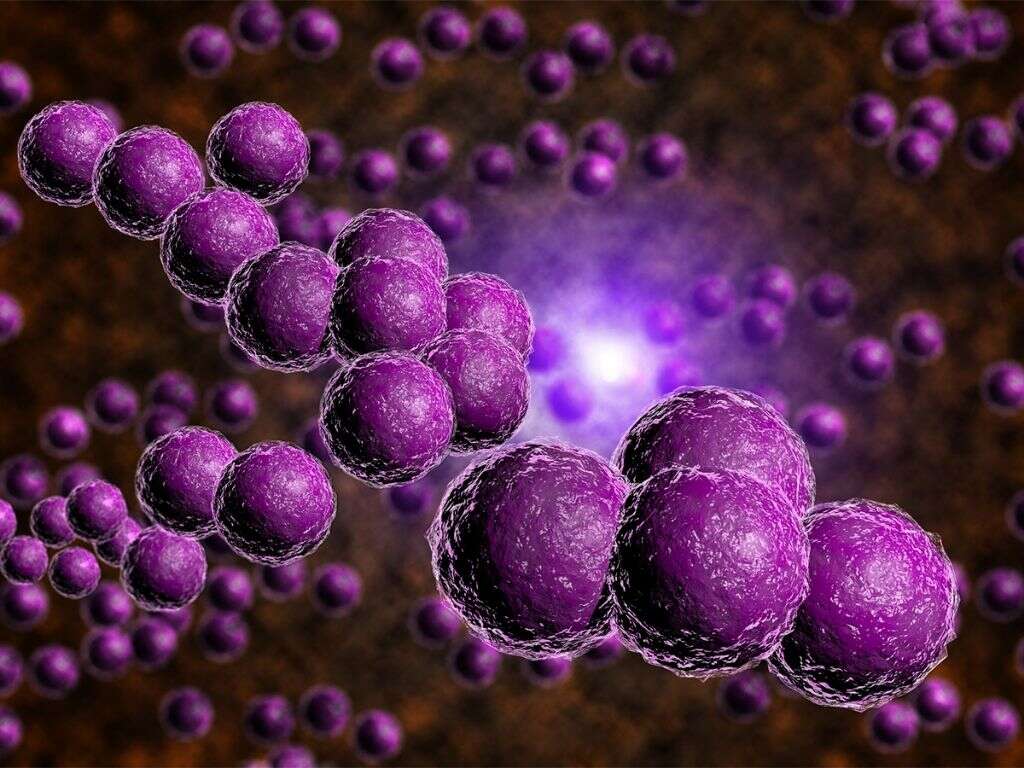
2. What Types of Bacteria Cause Skin Infections?
The skin can become infected with a wide range of bacteria. A large portion is caused by one of the many subspecies of either Staphylococcus or Streptococcus bacteria. Some bacteria have developed resistance to common antibiotics. Methicillin-Resistant Staphylococcus Aureus (MRSA) has become a public health problem as it becomes more common.
Impetigo is another relatively common bacterial skin infection that generally occurs on the face, legs, or arms of children. It can be caused by either Staphylococcus aureus or Streptococcus pyogenes. In some cases, both bacteria are present.
3. Can Parasites Cause Skin Infections?
In some cases, parasitic organisms cause skin infections. They burrow into the skin to feed and to lay eggs, which later hatch within the host. Some parasitic infections you may be familiar with are lice, scabies, and bed bugs.
Good personal hygiene can limit the risk of infection with a parasite; however, it does not guarantee you will stay bug-free. Most parasites are resourceful and can survive for a long time in the environment. That can make them very difficult to fully eradicate from your surroundings.

4. Who Is at Risk of Getting a Skin Infection?
There are several risk factors for skin infections. People with weakened or otherwise compromised immune systems are more likely to develop diseases of any type, including in their skin. Areas of broken skin, sores, or open wounds can increase your risk as well. They allow dirt and pathogens to penetrate the skin’s outer layer and enter the body.
Certain types of behavior can increase infection risk. Health care settings often harbor large amounts of bacteria. Some of these, such as MRSA, have developed antibiotic resistance, which makes eradication difficult. Areas with high heat and humidity, such as locker rooms and public showers, often contain funguses that lead to infection. If you spend time in these types of areas, then you should take extra precautions against skin infections.

5. What Are Common Signs of Skin Infection?
Most minor skin infections cause a similar set of symptoms. People often experience redness, swelling, and raised rashes at the site of infection. In some cases, the rashes manifest as blisters or pustules. In others, they can develop into abscesses or open sores.
Pain or itchiness is another common symptom of most skin infections. For many people, the discomfort is limited to the immediate area of infection. However, if the infection spreads or gets into the bloodstream, pain and inflammation may manifest in other parts of the body.

6. When Should You See a Doctor for a Skin Infection?
Skin and soft-tissue infections (SSTI) can be classified into uncomplicated SSTI and complicated SSTI. Most cases of uncomplicated SSTIs are associated with folliculitis and superficial cellulitis. On the other hand, complicated SSTIs include infected burn wounds, large abscesses, necrotizing fasciitis, and many others.
A healthcare professional should always be consulted to assess the extent of the infection and to administer proper treatment in order to prevent further complications. If left untreated, a simple folliculitis could turn into a more serious infection that might require intravenous antibiotics. If you experience systemic symptoms like fever and malaise, it could be a sign that the infection has spread and medical attention is necessary.

7. How Are Skin Infections Diagnosed?
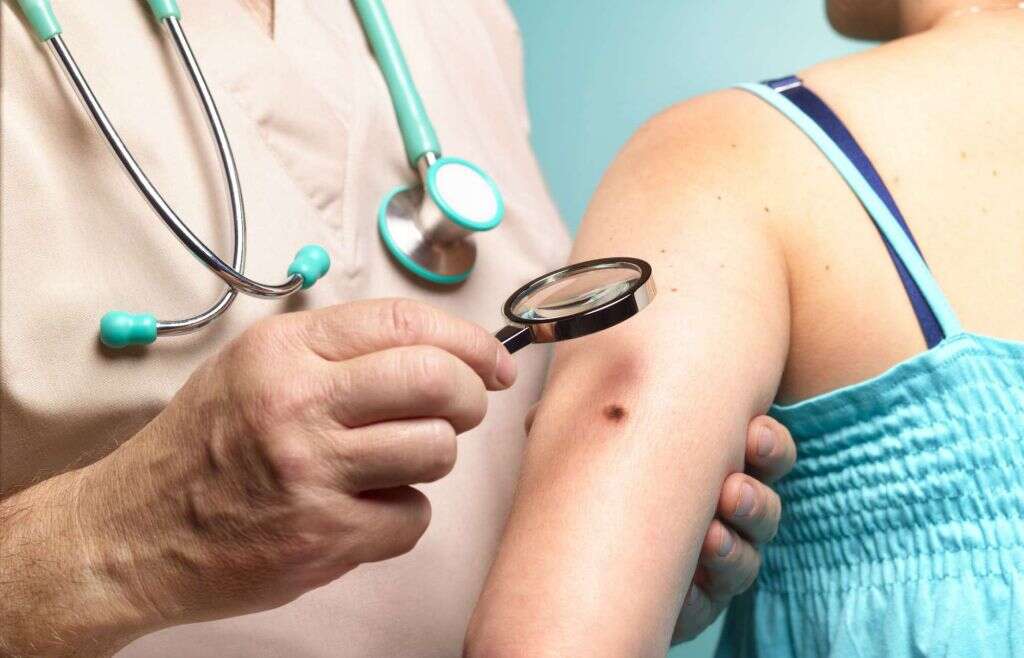
The doctor will perform a physical examination to look for signs of infection. In most cases, the rash and other external symptoms will be enough to result in a successful diagnosis. This is because many conditions produce predictable symptoms such as a particular type of pustule, rash pattern, or discoloration.
However, some infections may need to be biopsied or scraped for further analysis. The sample will be collected from the affected skin and taken to a lab. There, technicians can determine the exact cause of the infection so that a proper treatment plan can be developed.
8. Are Skin Infections Contagious?
Skin infections can be contagious. You should minimize contact with others to avoid spreading the underlying cause. Treatment with an appropriate medicine can reduce its infectiousness and the chance of you spreading it.
If you think you have come into contact with a pathogen that could cause an infection, wash the affected area as soon as possible. It also helps to keep any open wounds or patches of broken skin protected so infections cannot penetrate the skin.

9. How Are Skin Infections Treated?
The level of treatment necessary will largely depend on the severity, type, and location of a skin infection. Many minor cases can be treated with over the counter medications, such as antibiotics for bacterial infections and antifungal creams for fungal infections. However, there are times when a condition requires more targeted treatment.
Infections that have spread beyond the skin or that have entered the bloodstream can cause serious health complications. They require treatment with an appropriate oral or intravenous medication. The type of drugs will be determined based on the specific microbes that are present. Options include antibiotics, antifungals, anti-parasitic drugs, or a broad-spectrum antimicrobial.

10. Can Skin Infections Be Fatal?
For most people, skin infections are a minor inconvenience. However, they can actually be fatal. Some bacteria, such as certain strains of Staphylococcus, cause areas to become necrotic. This can lead to the amputation of an affected limb or the introduction of additional pathogens through the resulting open sores.
MRSA is an especially dangerous bacterium because it is resistant to common treatments. It is also known to strike patients in health care settings, where there is an increased likelihood of other complicating factors.