Orchitis Definition, Symptoms and More
 Article Sources
Article Sources
- 1. 'Orchitis.' Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Nov. 2020, www.mayoclinic.org/diseases-conditions/orchitis/symptoms-causes/syc-20375860.
- 2. 'Overview of the Male Anatomy.' Johns Hopkins Medicine, www.hopkinsmedicine.org/health/wellness-and-prevention/overview-of-the-male-anatomy.
- 3. 'Understanding How Testosterone Affects Men.' National Institutes of Health, U.S. Department of Health and Human Services, 25 Apr. 2016, www.nih.gov/news-events/nih-research-matters/understanding-how-testosterone-affects-men.
- 4. 'Orchitis: MedlinePlus Medical Encyclopedia.' MedlinePlus, U.S. National Library of Medicine, medlineplus.gov/ency/article/001280.htm.
- 5. Publishing, Harvard Health. 'Epididymitis And Orchitis.' Harvard Health, www.health.harvard.edu/a/to/z/epididymitis-and-orchitis-a-to-z.
- 6. 'Orchitis.' Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Nov. 2020, www.mayoclinic.org/diseases-conditions/orchitis/diagnosis-treatment/drc-20375865.
- 7. 'Orchitis.' Winchester Hospital, www.winchesterhospital.org/health-library/article?id=948960.
- 8. 'Testicular Torsion.' Mayo Clinic, Mayo Foundation for Medical Education and Research, 4 Apr. 2020, www.mayoclinic.org/diseases-conditions/testicular-torsion/symptoms-causes/syc-20378270.
- 9. 'Testicular Cancer: Symptoms, Causes, Diagnosis & Treatment.' Cleveland Clinic, my.clevelandclinic.org/health/diseases/12183-testicular-cancer.
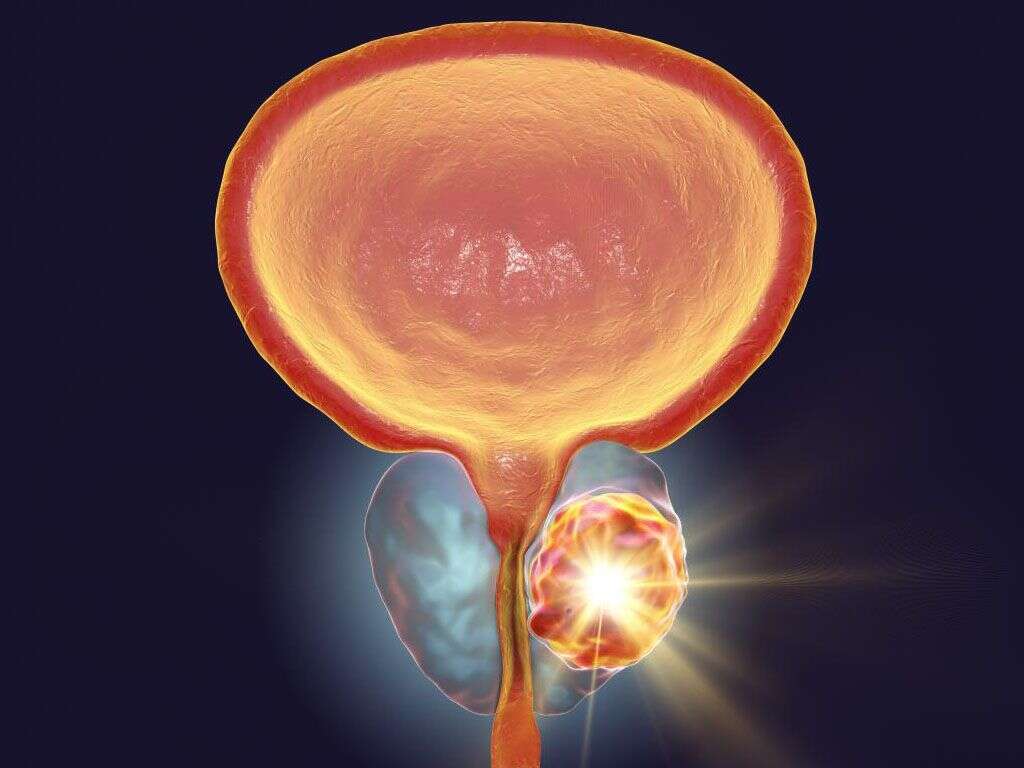
Orchitis occurs when one or both testicles become inflamed and painful.1‘Orchitis.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Nov. 2020, www.mayoclinic.org/diseases-conditions/orchitis/symptoms-causes/syc-20375860. Located inside the scrotum, the testicles produce sperm and the hormone testosterone. Testosterone plays a role in male development, helping to deepen the voice and regulating sex drive, sperm and red blood cell production as well as bone and muscle mass.2‘Overview of the Male Anatomy.’ Johns Hopkins Medicine, www.hopkinsmedicine.org/health/wellness-and-prevention/overview-of-the-male-anatomy.,3‘Understanding How Testosterone Affects Men.’ National Institutes of Health, U.S. Department of Health and Human Services, 25 Apr. 2016, www.nih.gov/news-events/nih-research-matters/understanding-how-testosterone-affects-men.
Epididymitis sometimes occurs simultaneously with orchitis. Epididymitis is an inflammation of the epididymis, a coiled structure behind the testicle responsible for sperm storage and transport. When orchitis and epididymitis are both present, the condition is called epididymo-orchitis. Causes, symptoms, diagnosis and treatment are the same for all three conditions.1‘Orchitis.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Nov. 2020, www.mayoclinic.org/diseases-conditions/orchitis/symptoms-causes/syc-20375860.

1. Orchitis Symptoms
A person with orchitis usually experiences pain, swelling and a heavy feeling in the affected testicle(s), and the area may appear red and feel warm. They may also have groin pain and swelling, and they may walk with a limp due to the pain. They may notice a clear, white or yellow discharge from the penis. Pain may occur during urination, intercourse or ejaculation, and blood may be present in their semen.
Fever and chills may be present, and the person may feel generally unwell. Nausea and vomiting may also occur.1‘Orchitis.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Nov. 2020, www.mayoclinic.org/diseases-conditions/orchitis/symptoms-causes/syc-20375860.,2‘Overview of the Male Anatomy.’ Johns Hopkins Medicine, www.hopkinsmedicine.org/health/wellness-and-prevention/overview-of-the-male-anatomy.,4‘Orchitis: MedlinePlus Medical Encyclopedia.’ MedlinePlus, U.S. National Library of Medicine, medlineplus.gov/ency/article/001280.htm.

2. Orchitis Causes
Viruses and bacteria cause orchitis, although in some cases the exact underlying cause is unknown. Mumps is the most common cause of viral orchitis in males. In approximately one-third of males who contract mumps after puberty, orchitis develops within a week of the onset.1‘Orchitis.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Nov. 2020, www.mayoclinic.org/diseases-conditions/orchitis/symptoms-causes/syc-20375860.
Sexually transmitted infections and infections of the urinary tract and prostate can lead to orchitis. Congenital abnormalities may increase the risk of orchitis, and it may occur following insertion of catheters or other medical equipment into the penis.1‘Orchitis.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Nov. 2020, www.mayoclinic.org/diseases-conditions/orchitis/symptoms-causes/syc-20375860.,4‘Orchitis: MedlinePlus Medical Encyclopedia.’ MedlinePlus, U.S. National Library of Medicine, medlineplus.gov/ency/article/001280.htm.

3. Risk Factors for Orchitis
People who haven't received a mumps vaccine are at risk of developing orchitis. Men who engage in behaviors that expose them to STIs also risk developing orchitis. These include having multiple sexual partners, engaging in sex with a person who has an STI and failing to use condoms.
Orchitis is more likely to afflict those with congenital urinary tract issues and men who often experience frequent urinary tract infections. Undergoing surgical procedures on the urogenital tract may also increase the risk of developing orchitis.1‘Orchitis.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Nov. 2020, www.mayoclinic.org/diseases-conditions/orchitis/symptoms-causes/syc-20375860.

4. Diagnosing Orchitis
To diagnose orchitis, the health care provider begins with a review of the person's medical history and symptoms before conducting a physical exam, which may include a rectal exam to check the prostate. They collect samples of urine, blood and any penile discharge for laboratory analysis.6‘Orchitis.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Nov. 2020, www.mayoclinic.org/diseases-conditions/orchitis/diagnosis-treatment/drc-20375865.
The provider may also order an ultrasound and a radionuclide scan to rule out testicular torsion, a painful condition in which the testicle becomes twisted and the blood supply is cut off.5Publishing, Harvard Health. ‘Epididymitis And Orchitis.’ Harvard Health, www.health.harvard.edu/a/to/z/epididymitis-and-orchitis-a-to-z.

5. Treatment for Bacterial Orchitis
Treatment for bacterial orchitis involves a course of antibiotics for the patient. If the bacterial infection was caused by an STI, the patient's sexual partners should receive antibiotic treatment as well. Taking over-the-counter pain medications and applying ice packs to the affected area may help alleviate pain.
Rest and using a strap to support the scrotum are also helpful. The tenderness may gradually dissipate a few weeks after treatment begins.6‘Orchitis.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Nov. 2020, www.mayoclinic.org/diseases-conditions/orchitis/diagnosis-treatment/drc-20375865.

6. Treatment for Viral Orchitis
Orchitis that's viral in nature usually resolves on its own. In this case, treatment is supportive with the goal of making the patient more comfortable. Bed rest is recommended. Elevating the scrotum and applying ice packs to the affected area may help alleviate discomfort. Over-the-counter nonsteroidal anti-inflammatory medications help mitigate pain while simultaneously reducing inflammation.
A person suffering from viral orchitis is likely to begin feeling better within 10 days, but scrotal tenderness may persist for several weeks.6‘Orchitis.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Nov. 2020, www.mayoclinic.org/diseases-conditions/orchitis/diagnosis-treatment/drc-20375865.
7. Complications of Orchitis
Infertility is a possible complication of orchitis. The condition may also result in inadequate production of testosterone. If just one testicle is affected by orchitis, these complications are less likely to occur.
In some cases, testicular atrophy may develop, with the testicle growing smaller in size. Other possible complications of orchitis include scrotal abscess, death of testicular tissue and formation of a fistula on the scrotum. Epididymitis may also develop.1‘Orchitis.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 6 Nov. 2020, www.mayoclinic.org/diseases-conditions/orchitis/symptoms-causes/syc-20375860.,4‘Orchitis: MedlinePlus Medical Encyclopedia.’ MedlinePlus, U.S. National Library of Medicine, medlineplus.gov/ency/article/001280.htm.
8. Preventing Orchitis
Since mumps is the most common cause of viral orchitis, receiving the MMR vaccine, which protects against mumps, measles and rubella, is the best way to prevent the disease.7‘Orchitis.’ Winchester Hospital, www.winchesterhospital.org/health-library/article?id=948960.
Practicing safe sex helps keep bacterial orchitis at bay. Utilizing condoms, avoiding sexual relations with people infected with sexually transmitted diseases and engaging in monogamous relationships help reduce the chances of becoming infected with bacteria that lead to orchitis.4‘Orchitis: MedlinePlus Medical Encyclopedia.’ MedlinePlus, U.S. National Library of Medicine, medlineplus.gov/ency/article/001280.htm.

9. Testicular Torsion
When a person presents with orchitis symptoms, a health care provider is likely to check for testicular torsion. The symptoms of the two conditions are similar, but a person with testicular torsion usually experiences sudden and extreme pain in the scrotum.
Testicular torsion occurs when the testicle twists and restricts blood supply to the testicle. Emergency surgery is usually necessary. Without prompt treatment, the testicle may become so badly damaged that it must be removed.8‘Testicular Torsion.’ Mayo Clinic, Mayo Foundation for Medical Education and Research, 4 Apr. 2020, www.mayoclinic.org/diseases-conditions/testicular-torsion/symptoms-causes/syc-20378270.

10. Testicular Cancer
Testicular cancer is another condition that has many symptoms in common with orchitis, although frequently the person notices a lump in the testicle as well. Using ultrasound results, the health care provider can identify abnormalities in the testicle that may indicate cancer. If cancer is present, the testicle will likely be surgically removed.
The most common cancer in men between ages 20 and 35, testicular cancer usually only affects one testicle, and it's usually curable.9‘Testicular Cancer: Symptoms, Causes, Diagnosis & Treatment.’ Cleveland Clinic, my.clevelandclinic.org/health/diseases/12183-testicular-cancer.