10 Optic Neuritis Symptoms
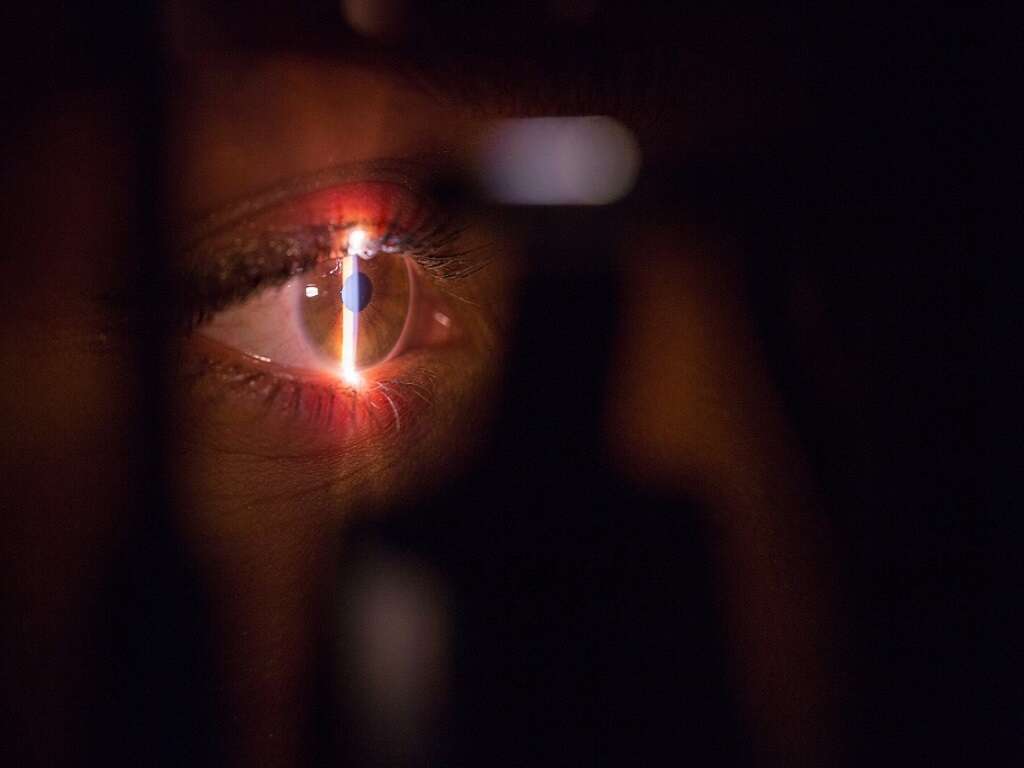
Optic neuritis is a condition where there is inflammation and demyelination of the optic nerve. It is often associated with multiple sclerosis (a demyelinating disease involving the nerve cells of the spinal cord and brain). Patients with multiple sclerosis often experience recurrent episodes of optic neuritis. Optic neuritis is a common early manifestation of multiple sclerosis. Those affected are often young females that may have a preceding viral illness. Long term studies have observed that up to 75 percent of female patients who initially present with optic neuritis ended up with multiple sclerosis. In some cases, optic neuritis can occur after a systemic viral infection. The diagnosis of optic neuritis can be achieved with the help of tests (erythrocyte sedimentation rate, thyroid function tests, antinuclear antibodies, rapid plasma reagin, mitochondrial deoxyribonucleic acid (DNA) mutation studies) to rule out other ocular conditions.
A magnetic resonance imaging (MRI) can also be helpful to assess the inflammatory changes, rule out structural lesions, and to look for white matter lesions in the central nervous system. Without treatment, the visual function usually improves after one to several weeks. However, permanent deficits in color, contrast, and brightness are common. Intravenous steroids and immunomodulators may be beneficial. Studies have indicated that there are approximately 4 to 5 cases per 100,000 individuals annually. Risk factors of optic neuritis include being Caucasian, female, and a young age (20 to 45 years old). If it occurs in children, it is usually due to an immune-mediated process (previous systemic infection or immunization).
Symptom #1: Loss of Vision
Loss of vision or visual impairment occurs when there is decreased ability to see to a point where it cannot be fixed using the usual means (such as spectacles). The loss of vision can result in difficulties with daily activities such as reading, driving, walking, socializing, and more.
Vision loss associated with optic neuritis usually involves only one eye, but it may also affect both eyes in rare cases. The vision loss usually resolves in a week or two.

Symptom #2: Blurred Vision
Blurred vision occurs when the image seen appears to be foggy or hazy. It is a common ocular symptom that can be caused by the use of atropine, presbyopia, cataracts, glaucoma, diabetic retinopathy, eye infection, eye inflammation, retinal detachment, stroke, optic neuritis, brain tumor, and more.
Optic neuritis in children may only have blurry vision as the only symptom.
Symptom #3: Pain in the Eye
Pain is an unpleasant and distressing feeling that is often due to an intense or damaging stimulus. Pain is one of the natural responses of the body to protect itself from damaging situations by withdrawing, resting, and allowing the affected area to heal.
In optic neuritis, almost all adult patients experience retro-orbital or eye pain that is aggravated by eye movement. The eye pain may be one of the earliest symptoms before loss of vision occurs.

Symptom #4: Reduced Night Vision
Reduced night vision refers to difficulty adjusting to dimly lit or dark environments. Patients start noticing that they have difficulty with tasks in poorly lit areas or having issues driving at night.
Reduced night vision can occur with nearsightedness, cataracts, retinitis pigmentosa, optic neuritis and more. In optic neuritis, the eyes have issues adapting and experience difficulty with glare and contrast.

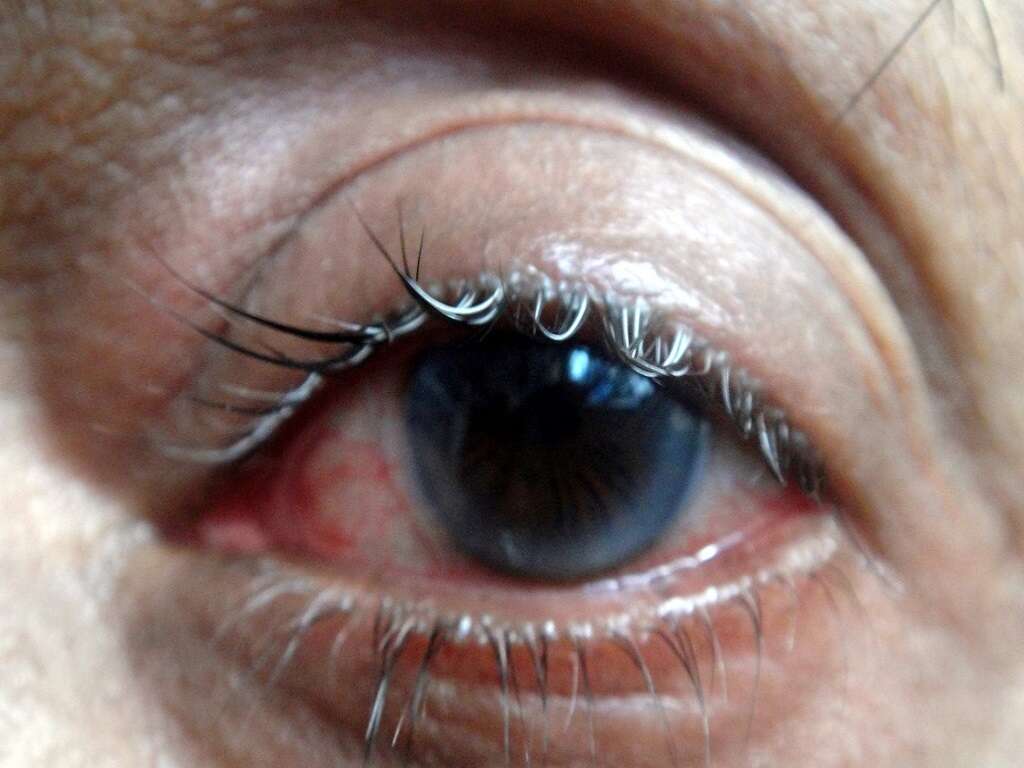
Symptom #5: Photophobia
Photophobia is the abnormal intolerance of light in the eyes. Patients complain of pain or discomfort in the eyes caused by light exposure. Photophobia can occur due to issues with the nervous system, eye conditions, genetic conditions, and other causes.
It occurs when excessive light enters the eye if there is corneal abrasion or inability of the pupil to constrict, lack of pigment in the iris due to albinism, traumatic brain injury, migraines, temporomandibular joint disorders, cataracts, uveitis, optic neuritis, and more.

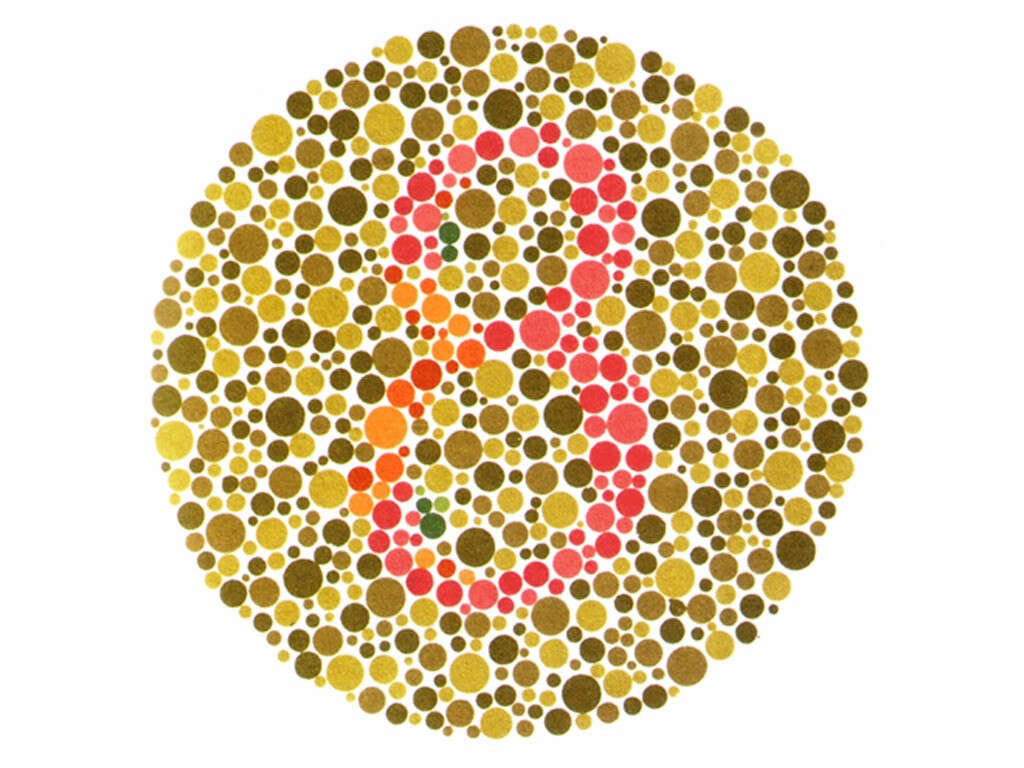
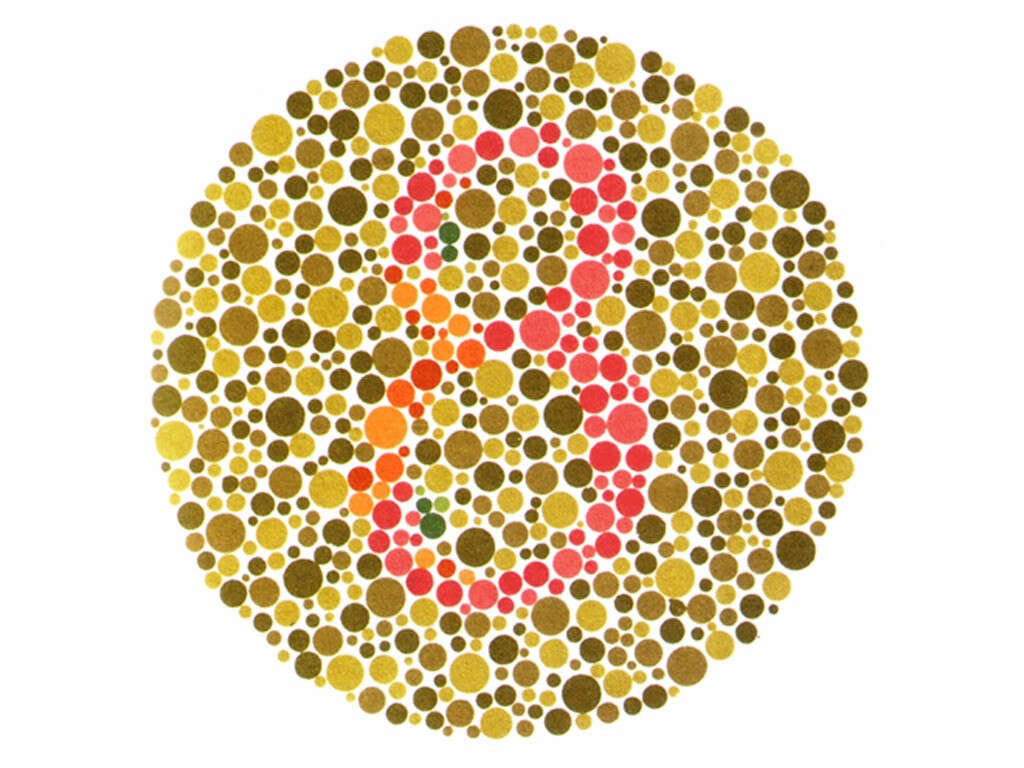
Symptom #6: Dyschromatopsia
Dyschromatopsia is defined as reduced or altered color vision. It occurs in almost if not all optic neuritis cases. Patients often describe it as a decrease in the vividness of colors especially shades of red. An Ishihara color chart can be used to evaluate the severity of reduced color vision.
Color testing is done separately in each eye to detect unilaterally affected cases. In optic neuritis, the severity of dyschromatopsia is far more than the loss of visual acuity. The reduced color vision is permanent.
Symptom #7: Uhthoff’s Phenomenon
Uhthoff’s phenomenon refers to the worsening of symptoms in multiple sclerosis and other demyelinating conditions when the body becomes overheated from exercise, saunas, hot tubs, fever, or hot weather. It is thought to be due to the effect of rising temperature on the conduction of nerves.
As the body temperature increases, nerve impulses are slowed or blocked in a damaged nerve. Symptoms resolve once the temperature normalizes. In optic neuritis, patients may describe worsening of vision or loss of vision when their body temperature increases or during exercise.

Symptom #8: Pulfrich Phenomenon
The Pulfrich effect is the situation where objects moving in a straight line appear to have a curved trajectory because of the different signal timings (conduction) between the two optic nerves. It can occur in cataract, multiple sclerosis, and optic neuritis.
This causes the patient to have difficulties during driving as they are unable to judge the paths of oncoming cars. Monocularly tinted spectacles in the daytime have been shown to reduce the symptoms of Pulfrich phenomenon.

Symptom #9: Headache
Headache refers to pain that occurs anywhere in the region of the neck or head. There are many types of headaches such as tension type headaches, cluster headaches, migraines, and more. Headaches are very common and can be caused by dehydration, fatigue, inadequate sleep, stress, side effect of medications, common colds, head injury, viral infections, and more.
It can be managed using pain medication such as paracetamol (acetaminophen) and non-steroidal anti-inflammatory drugs (NSAIDs). Headaches do not usually occur in adult optic neuritis but is commonly seen in pediatric optic neuritis.

Symptom #10: Flashing Lights
Flashing lights can refer to spots or pinpricks of light that the patient sees in their field of vision. It can appear wavy or like jagged lines. Some patients have described it as seeing “lightning streaks” or “shooting stars”. These flashes come from the eye or brain and are not present outside of the body. While occasional flashes are harmless, it should still be investigated to rule out serious issues.
Flashing lights can occur in conditions such as migraine and retinal detachment. Some patients with optic neuritis report seeing flickering or flashing lights with eye movements.