10 Causes of Dysphagia
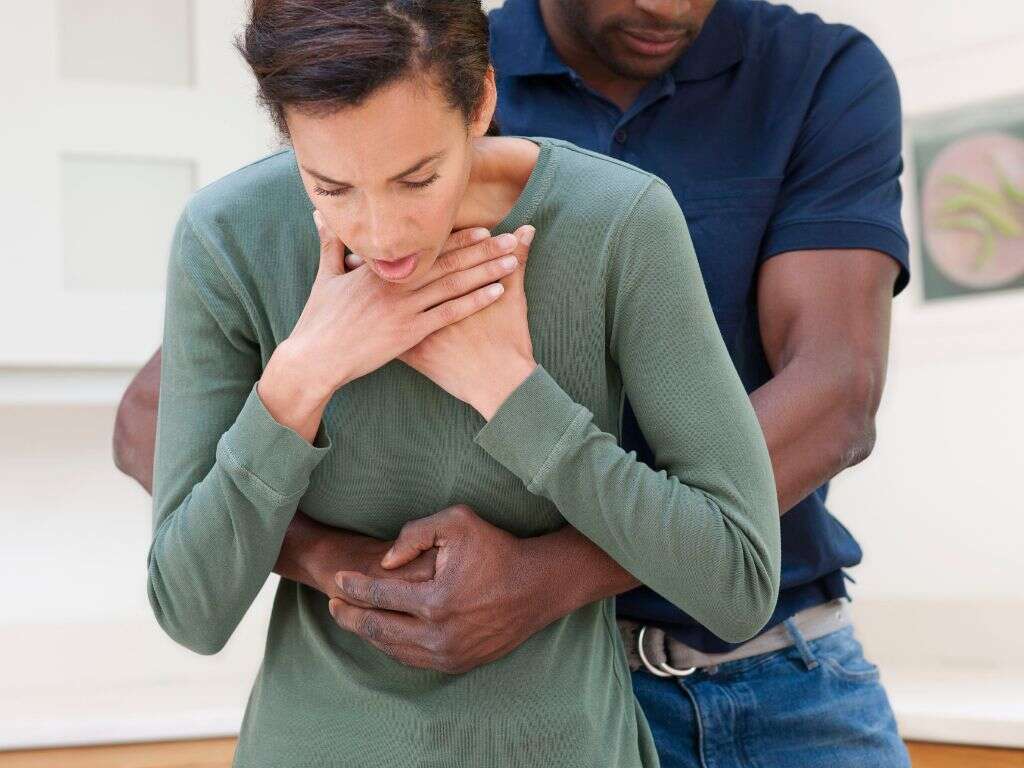
Dysphagia is a medical term that refers to difficulty swallowing or disruption in the swallowing process. This can include difficulty of passage of solids or liquids from the mouth to the stomach.
The process of swallowing has three phases: oral phase, pharyngeal phase, and esophageal phase. Dysphagia can be a symptom of several conditions, that may affect any of the three swallowing phases.
It is important to distinguish dysphagia from odynophagia, which refers to painful swallowing. When dysphagia is undiagnosed, those affected have a higher risk of pulmonary aspiration and aspiration pneumonia as solids or liquids can travel down the wrong passage (respiratory tract). Patients with dysphagia can also experience malnutrition, dehydration, and renal failure. Patients with dysphagia often experience other associated symptoms such as coughing, choking, inability to control food in the mouth, nasal regurgitation, and more.

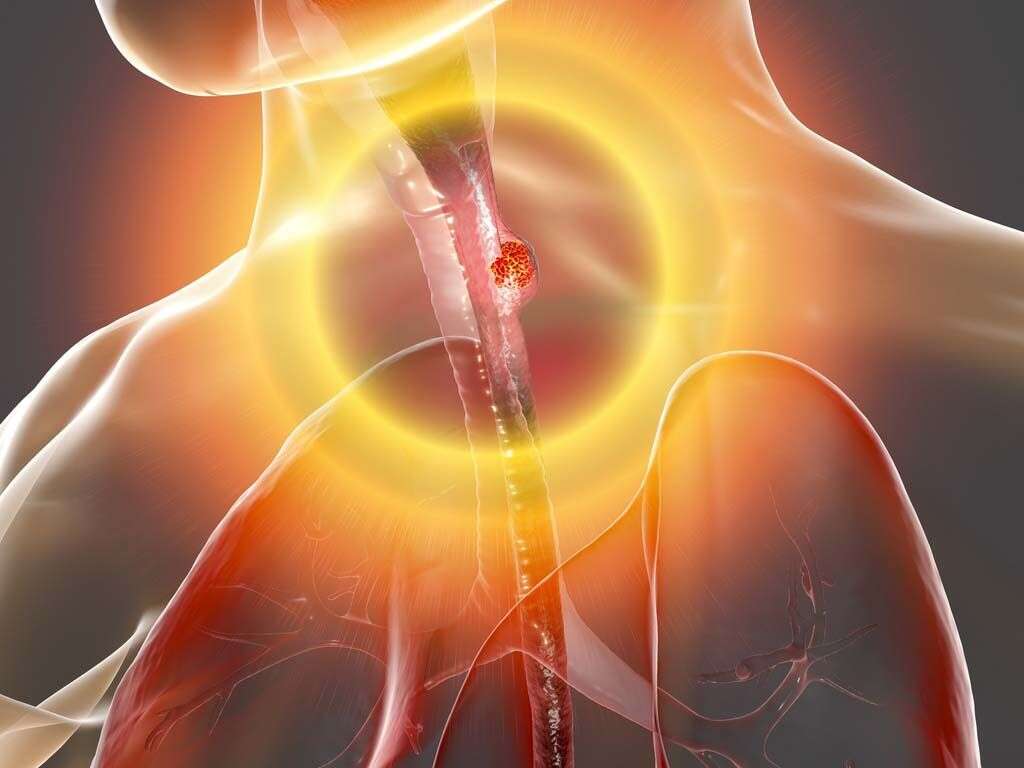
Cause #1: Esophageal Cancer
Esophageal cancer refers to cancer that originates from the esophagus. Symptoms of esophageal cancer usually include dysphagia, weight loss, hoarseness of voice, enlarged lymph nodes, odynophagia, coughing, and more. In these patients, dysphagia is the most common symptom, and it starts first for solids and progresses to include liquids.
Esophageal cancer can be generally divided into two types: adenocarcinoma and squamous cell carcinoma. Adenocarcinoma is usually found in the lower third of the esophagus with risk factors of obesity, acid reflux, and smoking tobacco, while squamous cell carcinoma occurs in the upper two-thirds with risk factors of consumption of very hot liquids, smoking tobacco and chronic alcohol consumption. Treatment is dependent on the stage and location of cancer.

Cause #2: Esophageal Varices
Esophageal varices occur when there are dilated submucosal veins present in the esophagus due to portal hypertension, which is a common consequence of cirrhosis. Patients with esophageal varices have a higher risk of bleeding.
Common signs and symptoms include dysphagia, blood in the vomit, having black or tarry stools, blood in the stools, loss of consciousness, and lightheadedness. Common associated symptoms due to cirrhosis would be jaundice, easy bruising, and more. Emergency care is directed at preventing further blood loss and stabilizing the patient.

Cause #3: Amyotrophic Lateral Sclerosis
Amyotrophic lateral sclerosis (ALS) is a motor neuron disease where there is death of neurons that function to control voluntary muscles. Patients with ALS may experience muscle twitching, stiff muscles, weakening muscles, difficulty speaking, dysphagia, and eventually difficulty breathing.
The diagnosis of ALS can be made based on the patients’ signs and symptoms with additional testing to rule out other potential causes. Currently, there is no cure for ALS.

Cause #4: Esophageal Web
Esophageal webs refer to thin membranes that may occur anywhere along the esophagus and can result in dysphagia and odynophagia. The esophageal webs are normal esophageal tissue that may cause obstruction in the esophagus. Congenital webs are usually seen in the middle and lower third of the esophagus. However, acquired webs are much more common and are usually seen in the postcricoid region (behind the cartilage that surround the trachea).
Esophageal webs are mainly associated with Plummer-Vinson syndrome. Diagnosis can be confirmed using a barium swallow test. Treatment involves endoscopic dilation of the webs.

Cause #5: Diffuse Esophageal Spasm
Diffuse esophageal spasm (DES) is a condition where there are uncoordinated contractions that occur in the esophagus. This results in regurgitation, dysphagia, and chest pain.
To evaluate the motor function of the esophagus, a test known as manometry can be performed to identify the abnormal patterns of contractions in the esophagus. It has also been observed that patients with DES tend to have higher incidences of anxiety and gastroesophageal reflux disease.

Cause #6: Zenker’s Diverticulum
Zenker’s diverticulum is also known as a pharyngeal pouch. It is a diverticulum of the esophageal mucosa (above the cricopharyngeal muscle). A diverticulum is an abnormal sac formed at a weak point in the wall of a specific part of the digestive tract. In this case, since it does not involve all the layers of the esophageal wall, it is a pseudo diverticulum. This condition occurs when the weakest portion of the pharyngeal wall balloons out when there is excessive pressure.
While some patients with Zenker’s diverticulum may be asymptomatic, some of the symptoms that may be present include regurgitation, dysphagia, halitosis, coughing, and more. A barium swallow and endoscopy help to confirm the diagnosis. This condition is most common among elderly patients.

Cause #7: Eosinophilic Esophagitis
Eosinophilic esophagitis is an inflammatory chronic allergic response in the esophagus involving eosinophils (a type of white blood cell). It can damage the esophageal tissue resulting in heartburn, dysphagia, vomiting, and impaction of food. While this condition is still not well understood, experts believe that food allergy may have a crucial role in the development of the condition.
Treatment of eosinophilic esophagitis includes removal of triggers or allergens and use of medication to suppress the immune response. Esophageal dilation may be required with endoscopy if the condition is severe.

Cause #8: Stroke
A stroke occurs when there is poor blood flow to the brain, which results in cell death. Stroke can be divided into ischemic and hemorrhagic. An ischemic stroke occurs when there is lack of blood flow while a hemorrhagic stroke occurs due to bleeding.
Patients with a stroke may experience the inability to feel or move a portion of their body, dizziness, difficulty understanding or speaking, dysphagia, loss of vision on one side, and more. The main risk factors of a stroke include high blood pressure, tobacco smoking, diabetes, obesity, atrial fibrillation, and more. Diagnosis can be supported using medical imaging. Treatment may involve surgery, thrombolysis, and stroke rehabilitation.

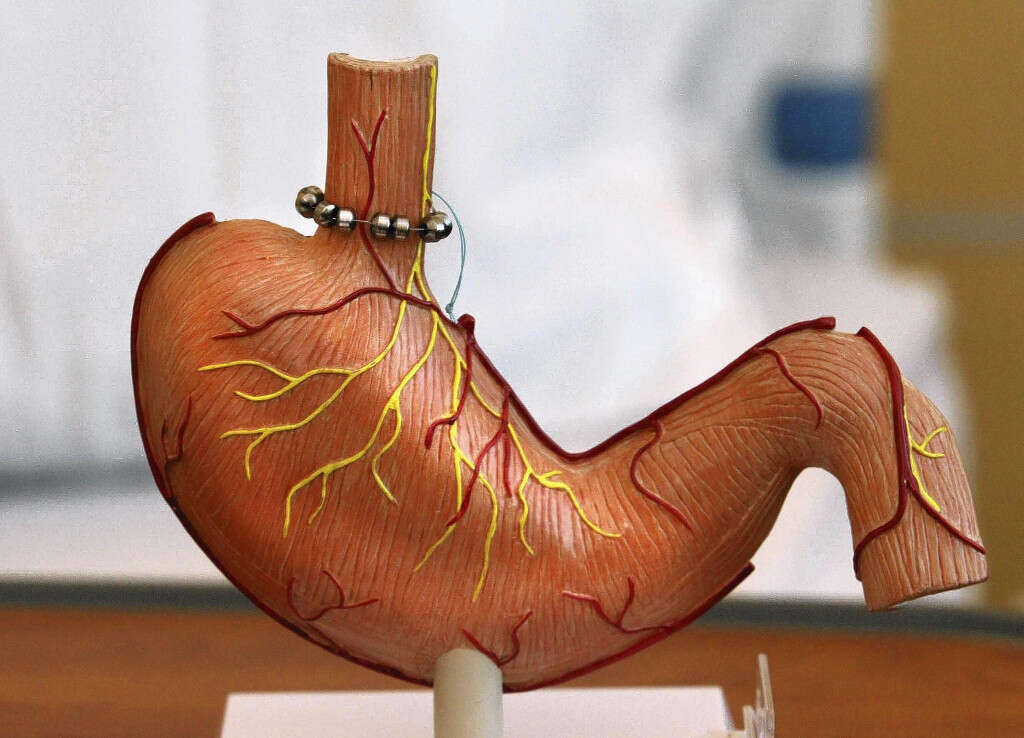
Cause #9: Gastroesophageal Reflux
Gastroesophageal reflux is a condition where the contents of the stomach (i.e. acid) backflow into the esophagus causing symptoms such as halitosis (foul breath), chest pain, heartburn, vomiting, bad taste in the back of the mouth, degeneration of teeth enamel, and dry cough. Chronic reflux leads to complications such as esophageal strictures (scar tissue that causes the narrowing of the esophagus), esophagitis (inflammation of esophageal lining), and Barrett’s esophagus. These complications can cause dysphagia.
Risk factors for this condition are smoking, obesity, pregnancy, hiatal hernia, and side effects of certain medications. Patients with this condition should try to make lifestyle changes and comply with the specific treatment prescribed by their physician.
Cause #10: Parkinson’s Disease
Parkinson’s disease is a chronic degenerative motor condition involving the central nervous system. The symptoms develop slowly with time. The earliest signs and symptoms of the disease often include rigidity, shaking, difficulty walking, and slowness of movements. As the disease develops, dementia, depression, and anxiety can also occur. Other associated symptoms include issues with sleep, and dysphagia.
While there is no cure for this condition, treatment is aimed at improvement of symptoms with anti-Parkinson medication.