What Is Systemic Scleroderma?
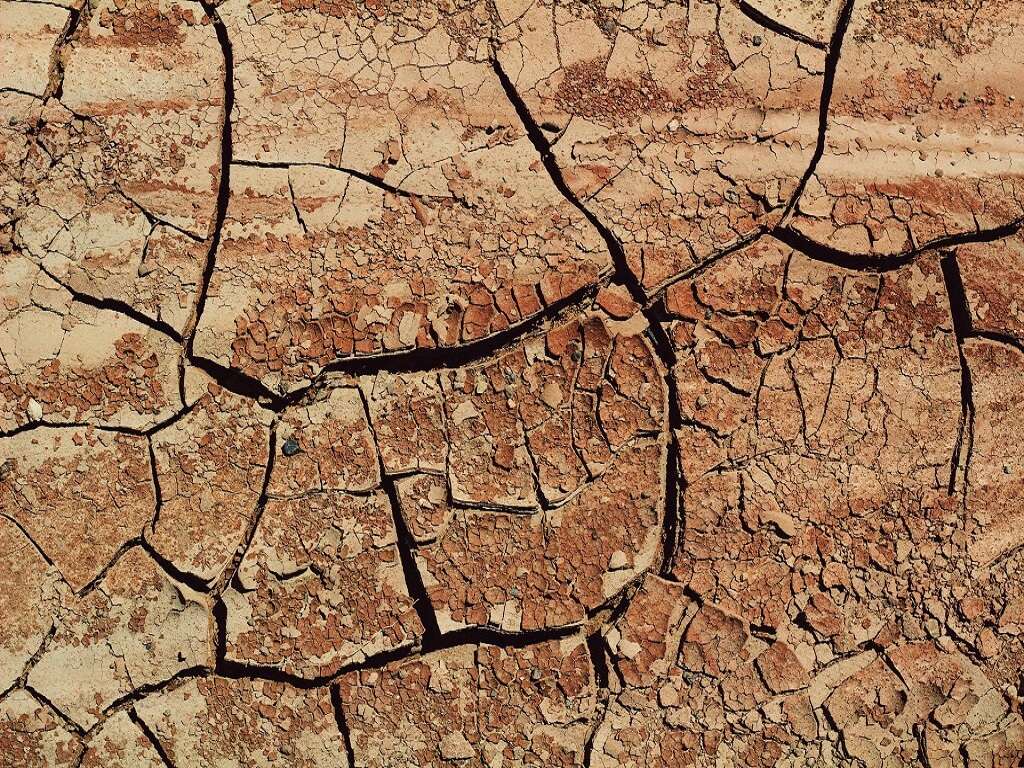
Systemic scleroderma is an autoimmune disease that causes an excess of collagen to develop in the skin or organs, resulting in the hardening and tightening of connective tissues. A healthy immune system helps to guard against viruses and infections by attacking foreign elements. Unfortunately, with autoimmune disorders, the immune system attacks the body’s tissues, causing a significant internal crisis.
Scleroderma is a Greek word meaning hard skin. The condition creates an autoimmune response where the body perceives an injury to the body’s tissues and organs, causing an excess of scar tissue to develop because of the overproduction of collagen. The disease can be incredibly dangerous, especially when it involves the internal organs. Therefore, to help you understand the condition, it is necessary to answer some of the most commonly asked questions

1. What Are the Signs and Symptoms of Systemic Scleroderma?
Systemic scleroderma has several possible symptoms, and they vary depending on the parts of the body that are affected. The areas of the body affected can be broken down into four categories: the skin, the digestive system, the fingers or toes and the heart, lungs or kidneys.
When scleroderma affects the skin, which occurs most frequently, a patient will notice hard patches on their limbs or body. While the number, size and location of these patches vary, they will typically have a shiny appearance because of the tightness of the skin. Also, patients may notice restricted movement.
When scleroderma affects the digestive tract, symptoms will depend on the location of the disease. For example, chronic heartburn or difficulty swallowing can be a result of scleroderma affecting the esophagus. If the disease is present in the intestines, patients may experience constipation, bloating, diarrhea and cramping. In some cases, scleroderma may prevent intestinal muscles from moving properly, eventually leading to malnutrition.
Raynaud’s disease is one of the earliest signs of scleroderma, and it affects the blood vessels in the fingers and toes. During cold seasons or times of emotional distress, the disease causes blood vessels to contract, possibly making the fingers and toes feel numb and turn blue.
In the most dangerous circumstances, systemic scleroderma might affect the heart, lungs or kidneys. If the function of any one of these organs is severely impaired, the disease can become life-threatening.

2. Are There Different Types of Systemic Scleroderma?
Systemic scleroderma is not a singular condition. There are three types of scleroderma, and they are defined by the affected tissues. Limited cutaneous systemic scleroderma is the first form of the disease and affects the face, hands and arms. Researchers have named this condition CREST syndrome because of the five commonly presented features: calcinosis, Raynaud phenomenon, esophageal motility dysfunction, sclerodactyly and telangiectasia.
The second form of this disease is called diffuse cutaneous systemic scleroderma. This version of the condition involves fibrosis of the skin, typically resulting in the hardening of large areas of the torso, upper arms and legs. Beyond affecting the skin, this form of the disease also affects the internal organs. Organ damage is often a serious concern with this type of systemic scleroderma.
The third form of the disease, systemic sclerosis sine scleroderma, is likely one of the most life-threatening. This version leads to fibrosis of one or more internal organs, but it does not affect the skin.

3. What Are the Complications?
As an autoimmune disease, scleroderma can affect many parts of the body. The severity and specifics will vary depending on a patient’s specific diagnosis. However, in general, there are seven areas that should be watched for complications: fingertips, teeth, digestive system, heart, lungs, kidneys and sex organs. The development of Raynaud’s disease is relatively common among systemic scleroderma patients. However, the restriction of blood vessels caused by this condition can be so severe as to permanently damage the tissue of the fingertips. Systemic scleroderma can also lead to severe tooth decay because of the shrinking and narrowing of the mouth. The tightness of the face resulting from skin fibrosis often makes dental hygiene difficult.
Also, there is less saliva produced among patients, which increases the rate of decay and tooth loss. Additionally, if the disease affects the digestive tract, patients may have internal discomfort and complications, leading to chronic heartburn, cramps and problems using the restroom. Scleroderma affecting the heart is dangerous and potentially life-threatening because it can lead to abnormal heartbeats and possible congestive heart failure. If the disease leads to scarring of lung tissue, lung function is compromised and individuals may struggle to breathe, possibly developing high blood pressure. Next, a common complications of scleroderma of the kidneys includes elevated blood pressure and increased protein levels in urine, which can lead to renal crisis and kidney failure. Last, the disease may inhibit sexual function. In men, it may lead to erectile dysfunction, and in women vaginal constriction and reduced output of sexual lubrication may be experienced.
4. Is This Condition Rare?
Systemic scleroderma is considered a rare autoimmune disorder, with significantly less than 1% of the population affected. However, there are still anywhere from 50 to 300 cases per 1 million people, and for them, the crisis is real and substantial.
Women are nearly four times more likely to be diagnosed with the condition than men, and there is no definitive explanation as to why that might be. Those affected should seek a specialist for treatment.

5. What Causes Systemic Scleroderma?
The underlying cause of systemic scleroderma is currently unknown. However, scientists speculate that it is the result of a combination of factors, including immune system problems, environmental triggers and genetics.
What researchers do understand is that the disease is a result of the accumulation and overproduction of collagen, which is a fibrous protein that makes up the connective tissue in the body. However, there are only theories as to why collagen is produced at such a rate, and the leading theory is that it is a result of an overactive and overprotective immune system.

6. Is This Condition Genetic?
Systemic scleroderma is not identified as a genetic disorder, with limited to no evidence suggesting a familial connection. However, there is a link between other autoimmune diseases like rheumatoid arthritis, lupus and thyroid disease, which indicates that there may be a hereditary component that is currently unknown.
While there may not be a definitive genetic link to a family history of the disorder, scientists have identified several genes that could point to the risk of developing the disease. The genes in question come from a group of genes known as the human leukocyte antigen complex. The HLA complex aids the immune system in distinguishing between the body’s natural proteins and proteins made by a virus, bacteria or other foreign invaders. When these genes mutate or form a variation not in line with the body’s normal functioning, then an individual could end up with an autoimmune disorder.

7. How Is Systemic Scleroderma Diagnosed?
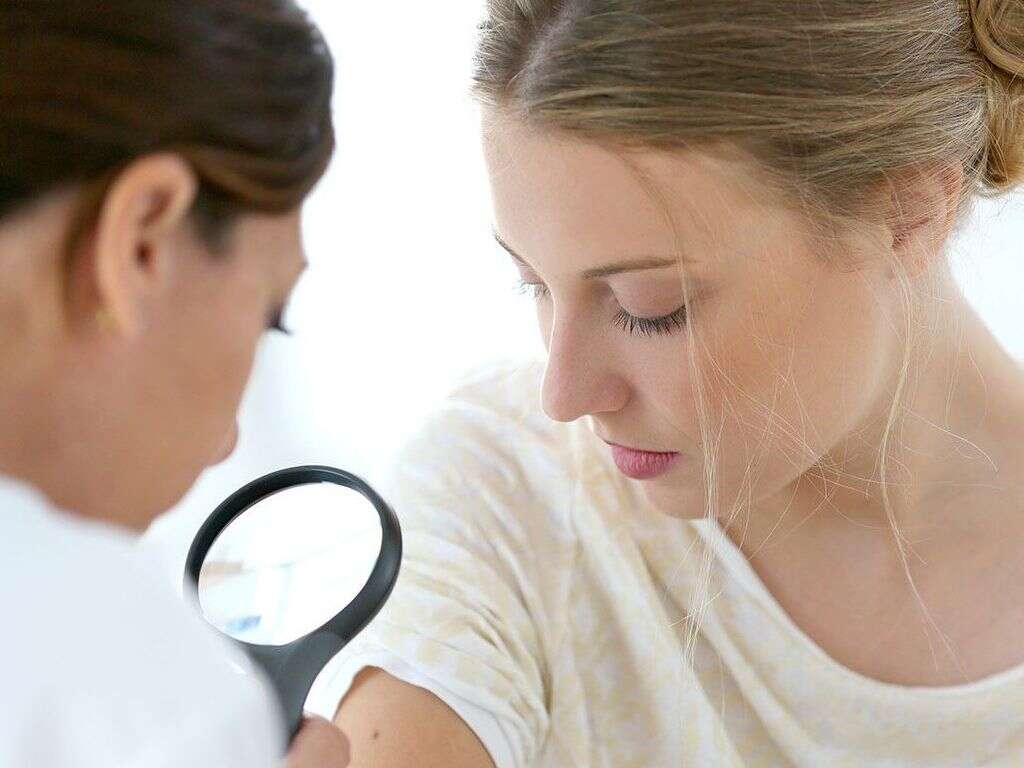
Systemic scleroderma is a disease of many forms. Diagnosing the condition is challenging and often involves a thorough physical exam. A doctor may perform a series of blood tests to check for elevated antibody levels, which may suggest an immune system response. If hard patches of skin are present, a physician may want to take a small sample to examine in a laboratory.
Beyond the standard tests and biopsies, a doctor may want to perform a series of imaging and organ-function tests to determine the health of vital organs.

8. Who Is More Likely To Be Affected by This Condition?
Systemic scleroderma is a rare condition that affects only a small percentage of the U.S. population. However, researchers estimate that, for every seven people with the disease, six are most likely women. For unknown reasons, systemic scleroderma is four times more likely to affect women than men.
The condition is more likely to develop in people between the ages of 35 and 50, although children and seniors may also develop the disease. Essentially, systemic scleroderma is still widely misunderstood because of a lack of available knowledge and research opportunity.

9. How Is Systemic Scleroderma Treated?
Systemic scleroderma is treated with a combination of medications, therapies and surgeries when needed. While no drug currently exists to stop or prevent the overproduction of collagen, there are medications, like steroid creams, blood pressure medicine and immunosuppressants, that can reduce and control the symptoms of the condition.
Additionally, physical and occupational therapists may work with the patient to help improve mobility and strength and manage pain. As a last resort, there are surgical options, including amputations and transplants, that may help relieve scleroderma complications.

10. What Can You Do To Manage the Symptoms?
If you have been diagnosed with systemic scleroderma, then you may be struggling with the uncertain nature of the disease. Beyond going to your doctor and following the treatment plan designed for you, you may also want to seek counsel from a therapist, religious leader or support group for other patients who may be going through the same or similar experiences.
Sometimes the hardest part of managing a disease is learning to accept it and find peace.