What Is Lazy Eye?
Amblyopia, or “lazy eye,” is a condition where there is decreased vision that cannot be corrected using contact lenses or prescription eyeglasses. It usually begins in infancy or early childhood. Although most cases affect only one eye, there are also some cases that affect both eyes.
Lazy eye is the most common reason of decreased vision in one eye among children and adolescents. With the proper intervention, most of the vision loss due to amblyopia is reversible or preventable. The recovery will depend on the age where treatment is started, the duration of abnormal eyesight, and maturity of the visual connections.
1. Mechanism
Although there are many types of amblyopia, it is believed that it is all due to the same basic mechanism. It is thought to be due to a developmental issue in the brain where the part that receives images from the lazy eye is not properly stimulated and, therefore, not able to develop to its full visual potential. This was confirmed by David H. Hubel and Torsten Wiesel who won the Nobel Prize in physiology or medicine in 1981. They were able to show the damage that occurs in kittens when there is visual deprivation during the critical development period. In humans, this is believed to be from birth to two years old. There are also some organic problems that can cause the persistence of a lazy eye even after the original condition has been treated and resolved.
2. Statistics
Based on available literature, the prevalence of amblyopia is estimated to range from 1% to 3.5% among healthy children and 4% to 5.3% among children who have ophthalmic issues. In the Visual Acuity Impairment Survey conducted by the National Eye Institute, amblyopia was reported to be the main cause of monocular (single eye) vision loss among adults between the ages of 20 to 70 years old.
There is no racial or gender preference. Lazy eye occurs during a critical time of visual development. The risk of amblyopia increases among children who have a positive family history, are developmentally delayed, or were premature during birth. This condition was first described in the 1600s and has caused many individuals to be ineligible as police officers and pilots.

3. Signs and Symptoms
Many patients with amblyopia, especially those who have a mild form, are usually unaware that they have this condition until they are tested at an older age. This is often due to their other eye being normal. On the affected eye, patients may have poor vision, low sensitivity to motion and contrast, and poor recognition of patterns.
Guardians may observe misalignment of the eyes (one eye may appear looking outward or inward while the other one is looking a different way) or fussing or crying when one eye is covered. Patients may have the two eyes not appearing to work together, often squinting, tilting of the head, have poor depth perception, and have abnormal results from vision screening tests.
4. Causes
Lazy eye can be caused by strabismus (misaligned eyes where one eye is favored strongly and fixation is not alternated) or anisometropia (where one eye is inhibited to eliminate the abnormal interaction caused by one focused and one defocused image).
Another cause of amblyopia is visual deprivation due to understimulation or disuse of the retina. This can be due to ptosis, cataract, surgical lid closure, and corneal opacities. Besides these three main causes, amblyopia may also be due to organic causes. Organic amblyopia is often irreversible due to an eye condition that limits the improvement of vision. Examples include retinoblastoma and toxoplasmosis chorioretinitis.

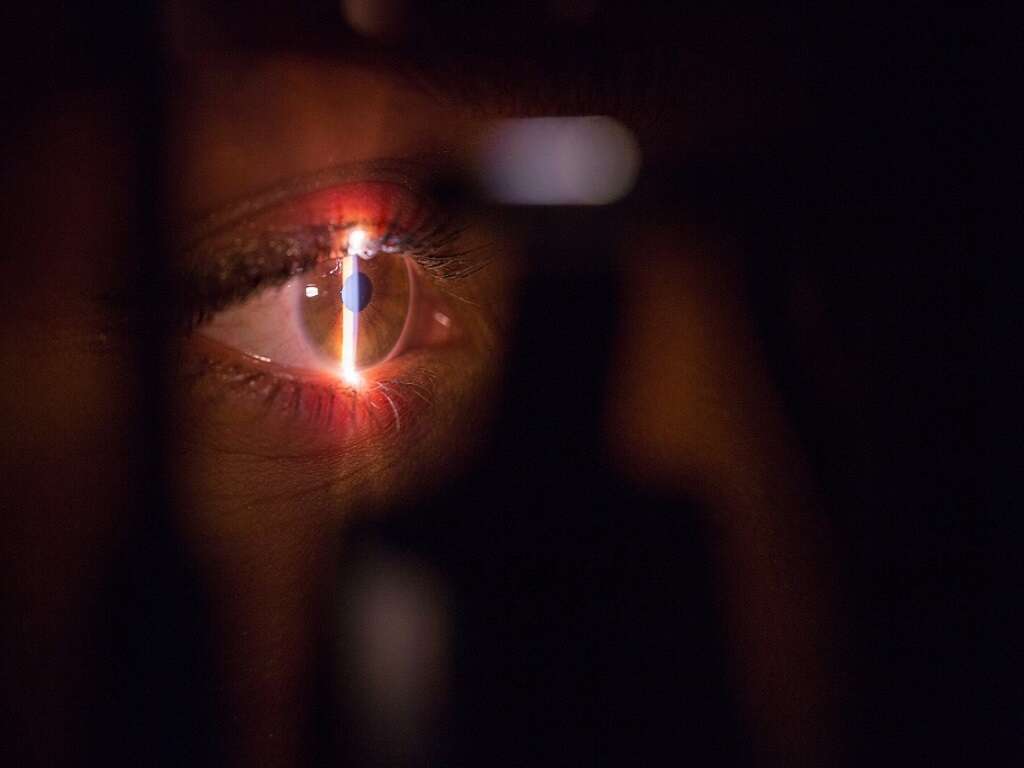
5. Diagnosis
Diagnosis can be achieved via the identification of decreased vison in one or both eyes only after other conditions are ruled out. Based on the Snellen chart, lazy eye can be defined as having a difference of having two lines or more in acuity. Since measurement of vision is difficult in young children, it can be estimated based on their reactions by covering one eye and observing their ability to follow an object.
Imaging using a computed tomography (CT) scan, magnetic resonance imaging (MRI) scan, and fluorescein angiography can also be useful to rule out other causes. Diagnosis and treatment should be done as early as possible so the vision loss is minimal. Screening for this condition should be performed for all children between the ages of 3 and 5.
6. Medical Care
It is important to first rule out an organic cause and treat any existing conditions such as cataracts. Congenital cataracts should be treated the first 2 months of life followed by treating refractive errors and anisometropia. An accurate correction for the lazy eye should be done next. All these should be done before occlusion therapy as there is a chance for vision to improve. Refractive correction has been found to improve amblyopia in 25% of patients. Occlusion therapy will then be performed by eye patching full time or part time. When there is no improvement of vision, it is important to consider poor compliance.
Besides adhesive patches, occluders on spectacles, adhesive tape on glasses, and opaque contact lens are also options that can be considered. Guardians should closely supervise children on occlusion therapy to make sure they do not peek. Older children may be enticed using a reward system while mittens and arm splints can be used in infants.

7. Surgical Care
After the reversal of amblyopia, surgical care for strabismus should be the next step. If surgical care is performed before amblyopia is corrected, it can be difficult to tell if amblyopia is present as the strabismus is no longer present to assess if the lazy eye is being used.
This can cause issues in nonverbal patients (young children who are still unable to communicate verbally). Correcting the strabismus before the amblyopia gives the guardians a false sense of security regarding the improvement of vision.
8. Trauma and Long-Term Monitoring
Young children who experience trauma to their eyes have a higher risk of occlusion amblyopia. This can occur if there is use of occlusive dressing, corneal opacity, vitreous hemorrhage, swelling of the eyelids, or cataract from trauma. Children who experience trauma to the eyes should be monitored closely, especially those who are nonverbal and under the age of 6 years old.
After completion of occlusive therapy, outpatient follow up should be continued as visual deterioration occurs in many patients. One study found that 25% of patients experience recurrence of amblyopia within one year after treatment. The risk of recurrence increases if the treatment was stopped suddenly instead of tapered.

9. Prevention
Studies have shown that vision screening programs are easy and can help reduce the cost and incidence of amblyopia as it helps with early detection and treatment. In a 9-year study where a volunteer photoscreening program is performed, 147,809 children were screened and 4.2% (6247) children were referred to professionals. Photoscreening is an automated technique where a special camera uses the red reflex to identify possible issues.
It is an easy and fast way to learn and is widely used in community group screenings. Out of these children, 24.3% were seen by an ophthalmologists while 76.7% were assessed by optometrists. In this study, the screening cost was about $9 per child. This shows that cost-effective screening is possible using a volunteer system. The method used for screening will depend on the child’s age and experience of the examiner.
10. Prognosis and Patient Education
It is estimated that after a year, 73% of patients are successfully treated after the first trial of occlusion therapy. However, studies have found that after 3 years, only 53% retain their level of visual acuity. Some of the risk factors for treatment failure are age (younger patients have a higher chance of success), presence of organic pathology, high anisometropia (unequal refractive power in both eyes), and the depth of amblyopia when therapy starts (mild cases respond better).
One study reported that patients who are successfully treated still have altered perception of images. Patients and their guardians should be educated regarding the importance of treatment and the consequences if adherence to treatment is poor. This is important as the outcome of treatment lies in the hands of the patient and their guardians.