What Is a Stent?
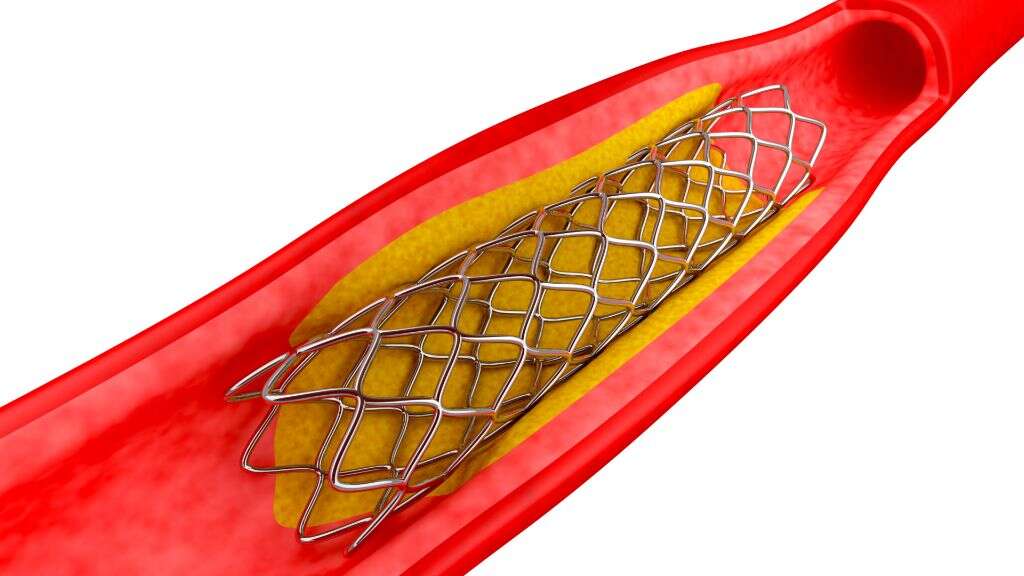
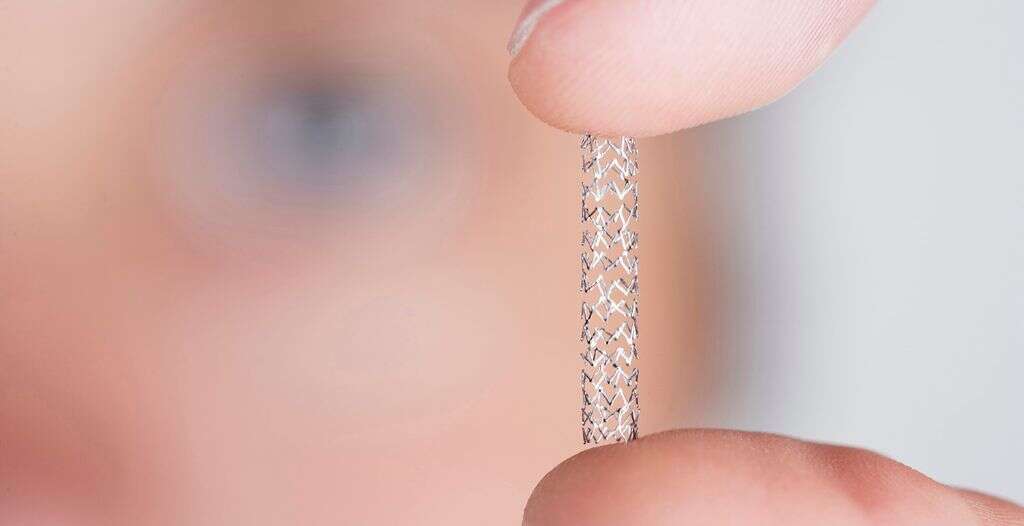
A stent refers to a tube made from plastic or metal that can be inserted into different parts of the body to help keep the passage or lumen open. The term “stenting” refers to the placement of a stent. By stenting a blocked passage, it restores the flow of blood or fluids. Stent grafts are stents that carry a full coating around their surface, providing full coverage to the vessel surface.
Stents can also be made from specialized fabric or coated with medication to provide additional benefits. There are many different types of stents for various purposes. Stents should be distinguished from shunts as stents maintain the passage while a shunt creates a new passage that never existed. While stents and shunts can be made using similar materials, they do not serve the same purpose.
1. History
In 1964, the concept of coronary angioplasty was first described using an implantable prosthetic. The first coronary angioplasty was then performed in 1977 during coronary artery bypass graft surgery. In the mid 1980s, coronary stents were developed and the first implantation of a stent occurred in 1986. In 1991, coronary stenting was used to treat acute myocardial infarction (heart attack).
The food and drug administration (FDA) then approved the used of stents for vessel closure in 1994. By 1999, the first drug-eluting stent was implanted. Between 2002 to 2004, Taxus and Cypher stents were approved in both the United States and Europe. The use of bioresorbable vascular scaffold was then approved in Europe in 2011.
2. Uses of a Stent
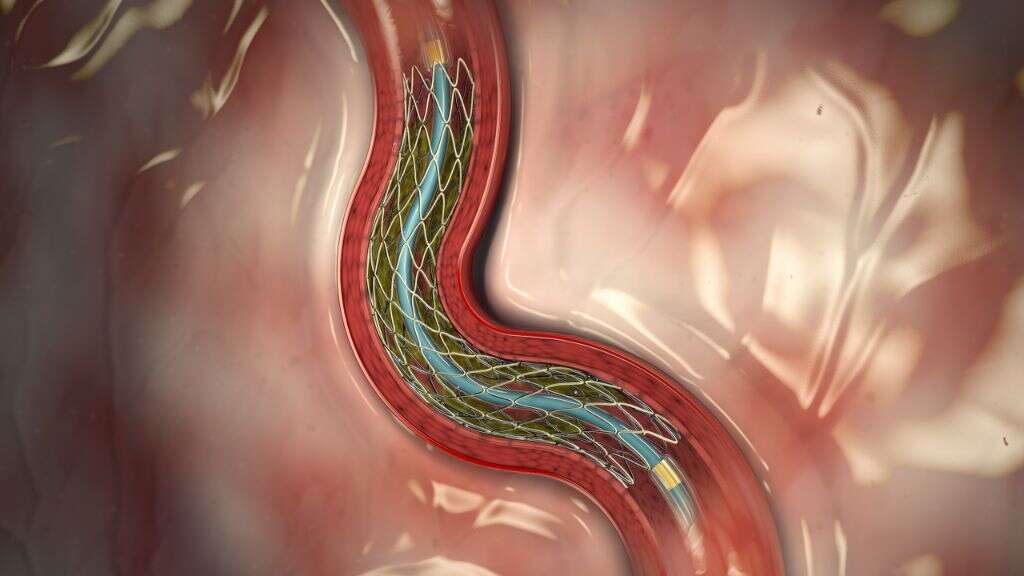
Stents can be used when a blood vessel is blocked by a plaque made of cholesterol and other substances that attaches to the vessel walls. This can be performed when the coronary artery is blocked to keep the vessel open. For example, during an emergency procedure for coronary artery blockage, a catheter is placed in the artery.
A balloon angioplasty is then performed to open the blockage and stent placed to keep it open. To prevent aneurysms from rupturing, a stent can also be placed. Stents can also be used to maintain the passageways in bronchi (small airways in the lungs), bile ducts (to maintain bile flow), and ureters (to carry urine from kidneys to the bladder).
3. Advantages and Disadvantages of a Stent
The placement of a stent only requires mild sedation. Since it requires no major incisions, there is minimal scarring. The placement of a stent is also a procedure that is relatively short. Compared to a coronary artery bypass surgery, stent placement surgery has a shorter recovery time with patients experiencing less discomfort.
Despite the many advantages, the procedure is not risk free. It can cause the formation of blood clots, which narrow the arteries again. This means that patients who have a stent will need to take blood thinning medication. When scar tissue or plaque forms in the area of the stent causing narrowing, this is known as restenosis. In these cases, the placement of another stent or surgery may be required.
4. Coronary Stents
A coronary stent is a small wire mesh tube that is placed in the coronary arteries (vessels that supply the heart) to keep obstructed arteries open and decrease their chance of narrowing again. Coronary stents are often used in percutaneous coronary intervention (coronary angioplasty) to help reduce symptoms such as angina (chest pain) or in the event of myocardial infarction (if applicable). It has been shown to improve survival and reduce complications (i.e. heart attack).
Two of the main complications of coronary stenting are re-occlusion due to proliferation of scar tissue, and restenosis. Restenosis occurs when a thick smooth muscle tissue develops inside the lumen. While the development is variable, it can cause restenosis in some cases.
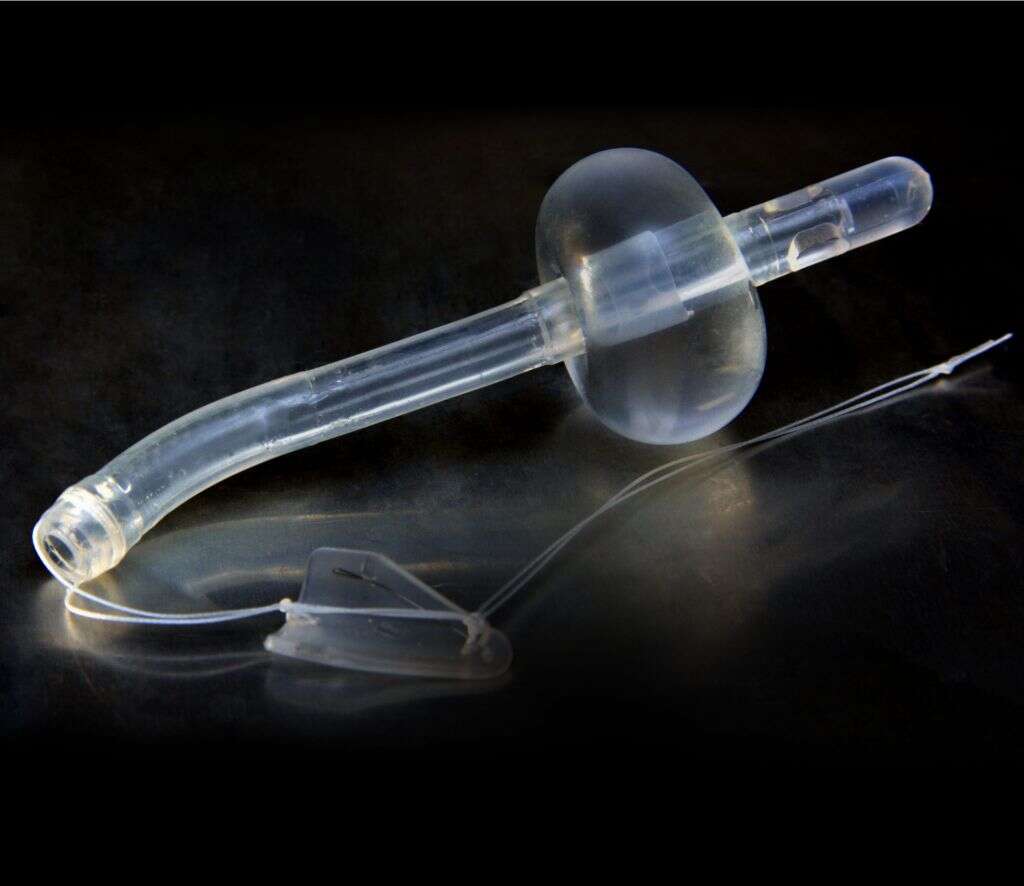
5. Ureteral Stent
A ureteral stent is a soft tube inserted into the ureter to maintain it open. The ureters are tubes made of muscle fibers that drain the urine from the kidneys to the bladder. This helps to treat or prevent obstruction of the urine flow from the kidney to the bladder. This is important as a blocked ureter can result in hydronephrosis (dilation of the kidneys due to the backflow of urine) and renal failure.
Ureteral stents can also be used as a temporary measure to prevent the kidneys from being damaged by a kidney stone until a procedure can be performed to remove the stone. It can also be used to hold the ureter open when it is compressed by a tumor in the surrounding area. Complications often include dislocation, blockage, and infection.
6. Prostatic Stent
A prostatic stent can be used to maintain the passageway of the male urethra to allow the passing of urine in cases of lower urinary tract obstruction and prostatic obstruction. Prostatic obstruction can occur in various conditions. It occurs most commonly in benign prostatic hyperplasia (BPH). However, obstruction may also occur after treatment of BPH, prostate cancer, or radiation therapy.
Prostatic stents can be permanent or temporary. A temporary stent can be placed just like a catheter and only requires topical anesthesia. The placement of a permanent stent is also performed as an outpatient procedure using topical, local, or spinal anesthesia. The prostatic stent may cause some discomfort and increase urinary frequency.
7. Esophageal Stent
An esophageal stent is placed to allow the patient to continue to swallow solids and liquids. It can be made from plastic, silicone, or self-expandable metallic stents for the treatment of esophageal cancer. The placement of an esophageal stent can be performed under conscious sedation or general anesthesia.
A catheter is first passed down the back of the mouth and the stent expanded against the esophageal wall to provide additional support. Besides esophageal cancer, it can also be used for gastric cancer, cancers that cause narrowing of the esophagus, ulcers, and post treatment with radiation. Although generally safe, it can cause issues such as bleeding, pain, tumor growth into the stent, gastroesophageal reflux, stent migration, and more.
8. Other Stents
Some of the other stents that are available include vascular stents often placed in the femoral, iliac, or carotid arteries; stent grafts used in endovascular aneurysm repair and to create fistulas for hemodialysis; biliary stents to maintain bile drainage from the pancreas, bile ducts, and gallbladder to the duodenum in conditions such as gallstones or ascending cholangitis; glaucoma drainage stents to reduce the pressure in the eye; and colonic stents, pancreatic stents, and duodenal stents.
Drug-eluting stents are stents that are coated with drugs to reduce the likelihood of narrowing. Clinical trials have shown that this reduces renarrowing cases to lower than 10%, resulting in decreasing the need for repetition of procedures.
9. Before Getting a Stent
There are certain tests and procedures required to prepare the patient for the procure.
Some of the tests may include a chest magnetic resonance imaging (MRI) scan, computed tomography angiography (CTA), magnetic resonance angiography (MRA), coronary angiography, fractional flow reserve, ultrasound, echocardiography, nuclear imaging, bronchoscopy, chest CT, and pulmonary function test. Blood tests can also be important. Patients should inform their doctors regarding any medical conditions, medications, supplements, or surgical procedures that they have had.
10. After the Procedure
After the procedure, most patients stay for a few hours in the hospital. Those with stent graft placement may need to stay in the hospital for a longer time. Patients will be informed regarding which medicines to take, when to resume normal activity, and when to make a follow-up appointment. Some of the medications that may be prescribed include mild painkillers (for pain at the incision site) and anticoagulant medication (to prevent clotting).
Possible complications of a percutaneous coronary intervention with stent placement include bleeding (from the catheter insertion site), an allergic reaction (to contrast agents used), infections, damage or dissection of the artery in question, and arrhythmias. Rare complications include stroke, myocardial infarction (heart attack), and death.