Large Intestine Function Overview
 Article Sources
Article Sources
- 1. Quigley, Eamonn M M. 'Gut Bacteria in Health and Disease.' Gastroenterology & Hepatology, Millennium Medical Publishing, Sept. 2013, www.ncbi.nlm.nih.gov/pmc/articles/PMC3983973
- 2. Rinninella, Emanuele, et al. 'What Is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases.' Microorganisms, MDPI, 10 Jan. 2019, www.ncbi.nlm.nih.gov/pmc/articles/PMC6351938
- 3. Sender, Ron, et al. 'Revised Estimates for the Number of Human and Bacteria Cells in the Body.' PLoS Biology, Public Library of Science, 19 Aug. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC4991899
- 4. Hsiao, William W L, et al. 'The Microbes of the Intestine: an Introduction to Their Metabolic and Signaling Capabilities.' Endocrinology and Metabolism Clinics of North America, U.S. National Library of Medicine, Dec. 2008, www.ncbi.nlm.nih.gov/pmc/articles/PMC4411945
- 5. Sears, Cynthia L. 'A Dynamic Partnership: Celebrating Our Gut Flora.' Anaerobe, Academic Press, 27 June 2005, www.sciencedirect.com/science/article/abs/pii/S1075996405000685
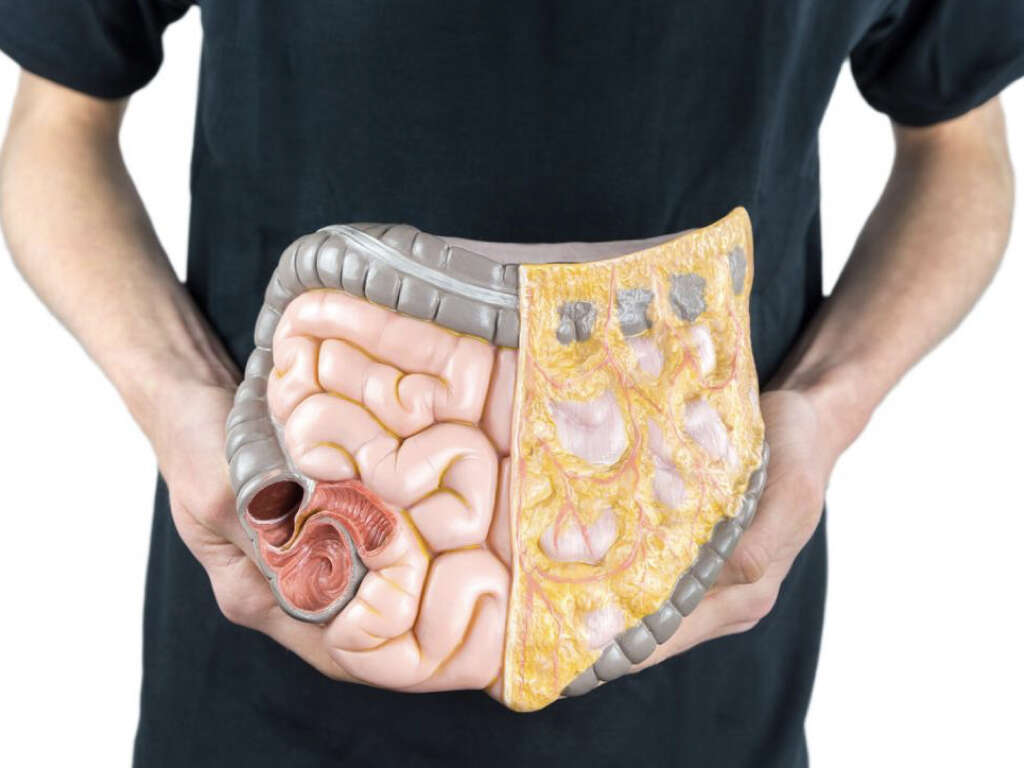
Also known as the gut, the large intestine reabsorbs water from food that hasn't been digested and compacts it into solid waste, which the body removes through defecation. It starts in the right iliac region of the pelvis, located below or at the waist. The bottom part of the small intestine joins the gut at this point.
Attached to the large intestine is the appendix, which has no known use and may become inflamed. The surface of the colon has three bands of 0.2-inch wide longitudinal fibers known as taeniae coli, which start at the appendix base, extending from the cecum to the rectum.
Additional Structures in the Large Intestine
Attached to the cecum's inferior surface is the appendix. It contains the least amount of lymphoid tissue and is critical to a person's immunity. If infectious food materials become trapped in the lumen, appendicitis might occur. The appendix may then have to be removed. However, its removal has no identifiable consequence to the body.
Epiploic appendages, also known as appendices epiploicae, are located along the sides of the gut's taeniae. These appendages are fat-filled peritoneum. The large intestines' characteristic features are the sacculations, also known as haustra, which don't exist in the small intestines.
Large vs. Small Intestine
The large and small intestines differ in their form in various ways. The colon is wider. The longitudinal layers of the muscularis are reduced to the taenia coli, which refers to the three strap-like structures. Simple columnar epithelium lines the wall of the large bowel.
Unlike the small intestines with its evaginations, the large bowel contains the intestinal glands, which are also known as invaginations. Even though goblet cells are present in the small intestines, they exist in much larger quantities in the large intestine.
Gut Bacteria and Fiber
The large intestine contains the human body's largest bacterial ecosystem, which plays several important roles. Several hundred species of bacteria live in the large intestine.1Quigley, Eamonn M M. ‘Gut Bacteria in Health and Disease.’ Gastroenterology & Hepatology, Millennium Medical Publishing, Sept. 2013, www.ncbi.nlm.nih.gov/pmc/articles/PMC3983973 These microorganisms perform various functions.
Some of these functions include forming products that the gut absorbs. For example, the bacteria in the large bowel metabolize undigested fiber and turn it into short fatty acids. The large intestine absorbs these acids through a process known as passive diffusion.
Gut Bacteria and Vitamins
Gut bacteria produces vitamins, including vitamin K and B, besides biotin through fermentation, which are absorbed into the bloodstream. This source of vitamins comprises only a small portion of the daily requirement, but the contribution can be significant in cases of low dietary vitamin intake.
A person who relies solely on the absorption of the gut-produce vitamins may suffer vitamin deficiency if they receive antibiotic treatment. This is because the antibiotics inhibit the growth of both the disease-causing bacteria and beneficial bacteria.3Sender, Ron, et al. ‘Revised Estimates for the Number of Human and Bacteria Cells in the Body.’ PLoS Biology, Public Library of Science, 19 Aug. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC4991899

Gut Bacteria and Immunity
Bacterial flora in the gut plays a role in the production of cross-reactive antibodies, which the immune system produces to fight against normal flora. However, these antibodies also prevent invasion and infection by other pathogens, as they can effectively fight them.
Bacteroides are the most prevalent bacteria in the gut. They are believed to play a role in the onset of colitis and colon cancer.2Rinninella, Emanuele, et al. ‘What Is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases.’ Microorganisms, MDPI, 10 Jan. 2019, www.ncbi.nlm.nih.gov/pmc/articles/PMC6351938 Another abundant gut bacteria is bifidobacteria, which are often recognized as friendly bacteria.
Gut Flora
The large intestine is a vast reservoir of microorganisms. To put it in context, the gut carries about ten times as many microorganisms as the number of cells, roughly 10 trillion, in the human body.3Sender, Ron, et al. ‘Revised Estimates for the Number of Human and Bacteria Cells in the Body.’ PLoS Biology, Public Library of Science, 19 Aug. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC4991899
According to some estimates, the bacteria in the large intestines have nearly a hundred times as many genes, in aggregate, as those present in the human genome.4Hsiao, William W L, et al. ‘The Microbes of the Intestine: an Introduction to Their Metabolic and Signaling Capabilities.’ Endocrinology and Metabolism Clinics of North America, U.S. National Library of Medicine, Dec. 2008, www.ncbi.nlm.nih.gov/pmc/articles/PMC4411945 Gut bacteria perform metabolic activities akin to those of an organ.

A Mutual Relationship
According to research, the relationship between human beings and their gut bacteria is not merely non-harmful or commensal, but rather one that is mutually beneficial.5Sears, Cynthia L. ‘A Dynamic Partnership: Celebrating Our Gut Flora.’ Anaerobe, Academic Press, 27 June 2005, www.sciencedirect.com/science/article/abs/pii/S1075996405000685 While it's possible to survive without gut bacteria, these microorganisms benefit the body in many ways.
Gut bacteria ferment unused energy substrates. They help prevent the growth of harmful, disease-causing bacteria and help train the immune system. Gut bacteria also produce vitamins and hormones that facilitate the storage of fat.
Passage of Food Into the Gut
The gut reabsorbs water from undigested food, compacts it into feces and stores it until it's defecated. When food passes from the small intestine into the large intestine, it stays there long enough for the gut bacteria to ferment it.
Gut bacteria break down some of the products of digestion in the small intestine. The large intestine absorbs some of these products, which include saccharides. Humans can digest three disaccharides at most.

Formation of Waste
The villi in the large intestine cannot absorb some food products, such as dairy or cellulose. Such food products are mixed with other bodily waste products and compacted into hard, concentrated feces.
The large intestine passes the feces into the rectum, where it is stored for a period. After some time, the feces are eliminated through defecation, which involves the contraction and relaxation of the anus. The anal sphincter regulates the exit of the waste material.
Defecation Reflex
In humans, defecation involves both voluntary and involuntary processes that generate enough force to evacuate solid waste material from the rectum. The rectal ampulla temporarily stores the waste. Thereafter, the accumulation of a sufficient amount of fecal waste triggers the defecation reflex.
The relaxation of the internal anal sphincter sends a signal to the brain and triggers the urge to defecate. Prolonged delay of defecation may cause constipation. During defecation, voluntary relaxation and contraction of the anal sphincter ejects waste material from the body.