10 Detached Retina Symptoms
 Article Sources
Article Sources
- 1. Common Eye Disorders and Diseases. (2020, June 03). Retrieved December 16, 2020, from https://www.cdc.gov/visionhealth/basics/ced/index.html
- 2. Pitcher, J., MD. (2017, July 01). Traumatic Retinal Detachment in Younger Patients. Retrieved December 16, 2020, from https://www.retinalphysician.com/issues/2017/july august-2017/traumatic-retinal-detachment-in-younger-patients
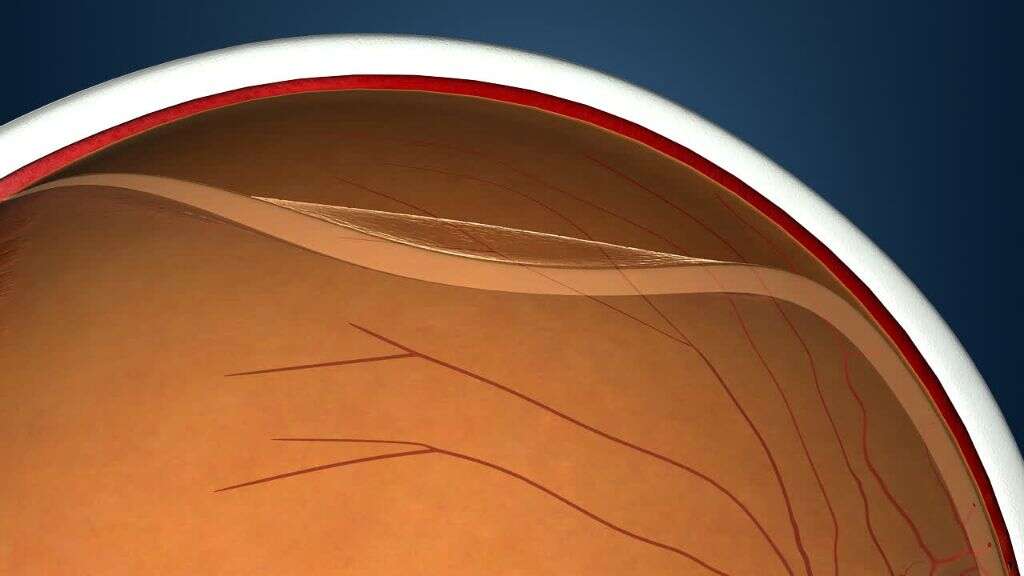
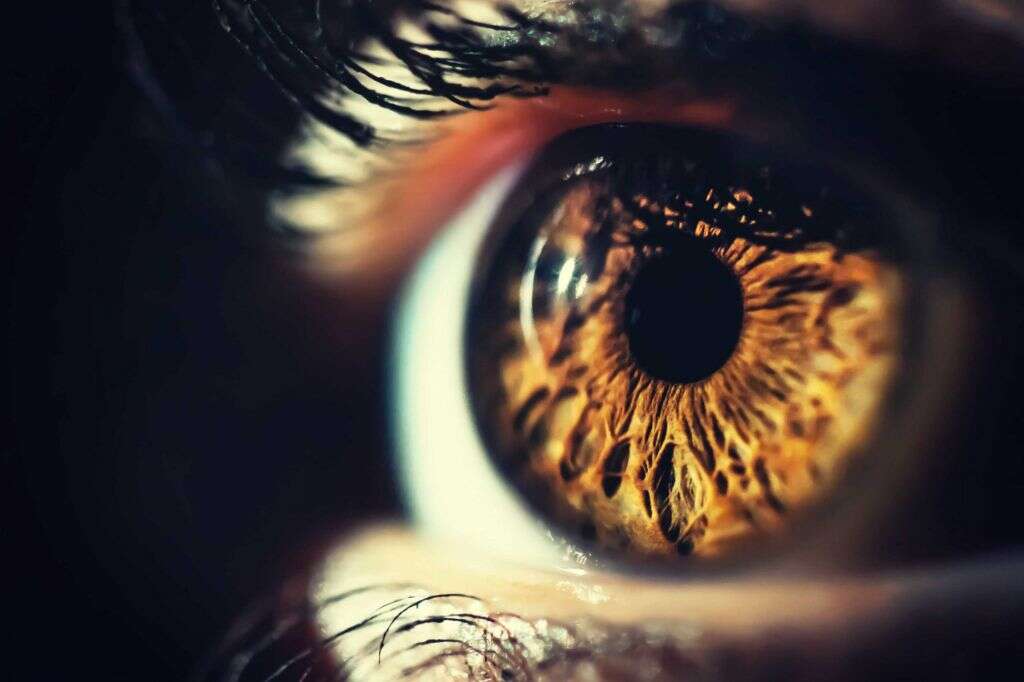
The retina is the light-sensitive layer at the back of the eye that contains cells that receive and organize visual information. These special cells, known as rods and cones, enable us to see by sending nerve impulses through the optic nerve into the brain. It is there where the visual image finally materializes. Importantly, the retina adheres to the back of the eyeball with the help of a gel-like material known as the vitreous. Unfortunately, as we age, the vitreous can change shape and tug on the retina. Retinal detachment can occur when the retina is pulled and separated from the back layer of blood vessels that supply it with oxygen.
Retinal detachment can have many possible causes including aging, trauma, and metabolic diseases (i.e. diabetes). Moreover, factors like aging (over the age of 40), a family history of retinal detachment, refractive errors (nearsightedness), previous eye surgery, and previous eye injury can greatly increase the risk of retinal detachment.
Importantly, retinal detachment is a time-critical emergency because it can permanently alter vision or cause the loss of vision entirely. If a retinal detachment is diagnosed after a retinal examination, surgical treatment will likely be required to repair the defect. Here are 10 possible signs and symptoms of a detached retina.
1. Gradually Reduced Side Vision
Peripheral vision, also known as side vision, gives us the ability to perceive objects that are out of our direct line of vision (central vision). Because of peripheral vision, we can notice things around us without the need to turn our heads or move our eyes. Interestingly, peripheral vision covers 100 degrees of a normal visual field of 170 degrees around. This type of vision is the result of different nerve cells and rods located outside of the macula (the region of keenest vision in the retina).
Peripheral vision loss is a common symptom among people with retinal detachment. It usually starts gradually, during the course of several days or weeks, even before retinal detachment is fully established. However, reduced side vision is not exclusive of retinal detachment given that other ocular diseases or injuries can cause it. For instance, glaucoma, retinitis pigmentosa, optic neuritis, and strokes can also cause peripheral vision loss.
2. Photopsia
Photopsia describes a sensation of flashing lights, usually in the peripheral part of the vision. Flashing lights can occur when the back of your eye (retina) is stimulated by something within rather than by the light that enters the structure. Typically, this visual disturbance has a sudden and brief onset; however, it can also become permanent. Moreover, depending on its cause, this symptom can affect one or both eyes simultaneously.
Photopsia can sometimes be normal; however, it may also be a sign of a retinal tear or the start of a retinal detachment. Since there is no way for a person that experiences this symptom for the first time to tell if it is normal or pathological, getting checked with a professional is recommended.

3. Floaters
As we get older, it is not uncommon to experience tiny dark shapes that occasionally float across our vision. These are known as floaters and they can take many forms, including threads, black dots, cobwebs, and lines. Floaters can be a result of normal changes in the eyes, so they often don’t require treatment. For instance, they can be caused by debris in the vitreous body (the gel that fills the space between the lens and the retina) that cast shadows onto the retina.
As mentioned, some people may have some floaters in their vision regularly; however, if these change and/or new ones appear (usually in large numbers) it can be a sign of a serious condition such as retinal detachment. Other possible causes of floaters include eye infections, eye injuries, inflammation of the eye (uveitis), retinal tear, and vitreous detachment.
4. Ring-Shaped Floaters
Floaters are tiny dark shapes that float across the vision. They can result from normal changes in the eyes; however, they can also be a sign of serious problems. Moreover, floaters can have many forms; which can sometimes vary depending on their cause. Most floaters are tiny and don’t interfere much with vision. However, in certain conditions, larger floaters can appear.
Floaters that appear suddenly and are large and circular can be a sign of a condition known as posterior vitreous detachment (PVD). In PVD the gel-like substance (vitreous), which normally fills the whole volume of the eye, shrinks and separates from the retina. When the vitreous finally separates from its annular attachment around the optic nerve (Weiss ring), a ring-shaped floater can appear in the center of the vision. Importantly, retinal detachment is a common complication of PVD; thus, it is not uncommon for these floaters to appear in this condition.
5. Blurred Vision
Blurred vision is an ocular symptom that can have many causes. When it occurs, your vision becomes less precise and you might experience difficulty to see fine details. Certainly, the primary cause of blurred vision is refractive errors such as farsightedness, nearsightedness, and astigmatism. However, blurry vision can also indicate more serious eyesight problems.
Retinal detachment is an important cause of blurred vision because it can cause permanent loss of vision if untreated. Before the detachment occurs, it is not uncommon to experience visual disturbances that can take the form of blurriness. Hence, if you develop sudden blurry vision with any of the other symptoms of retinal detachment, you should have your eyes examined immediately.
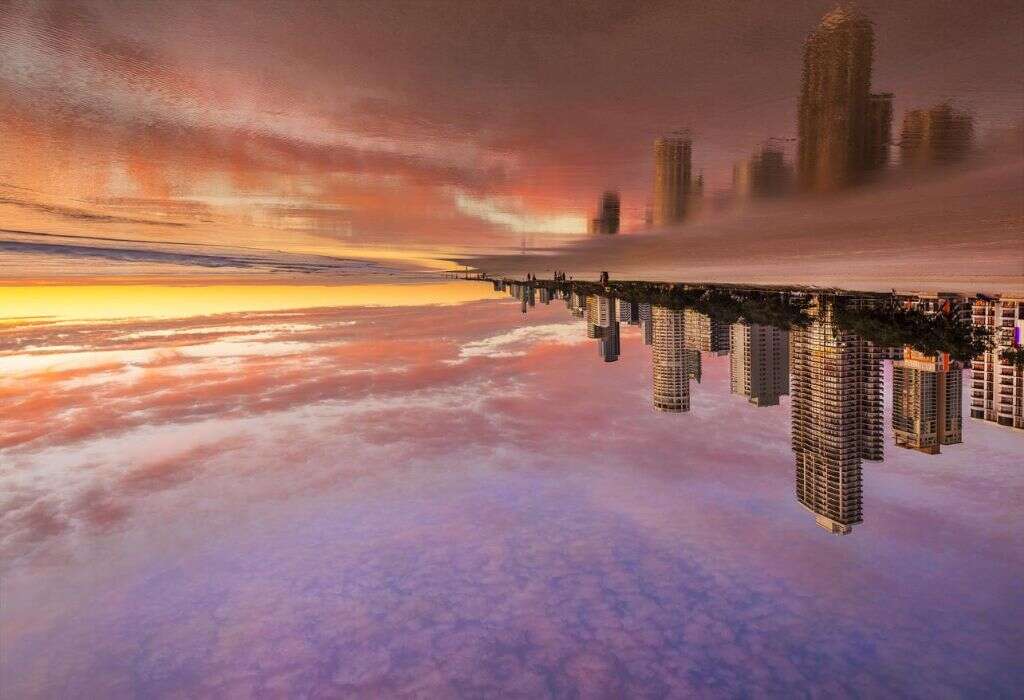
6. Metamorphopsia
Metamorphopsia is a visual symptom that refers to the perception of linear objects as curved or discontinuous, as seen by the patient. For instance, lines of text on a book can appear bent or wavy when reading them.
Metamorphopsia can be seen in a variety of ophthalmologic conditions, but it is most common in diseases that involve the macula (the region of keenest vision in the retina). For example, age-related macular degeneration can cause metamorphopsia. Importantly, certain types of retinal detachment can also cause this symptom. Additionally, metamorphopsia may persist or appear after retinal reattachment surgery.
7. Shadow or Dark Curtain in Vision
If the retina begins to detach and lose its oxygen supply, the detached areas may cease to work properly. As a consequence, the affected person’s vision may become partially blocked by grey or dark shapes that move across or on the edge of the visual field. This phenomenon is commonly reported as a curtain-like shadow, and it is a frequent symptom among people with retinal detachment.
As retinal detachment progresses, and more of the retina detaches, the curtain-like shadow will continue to move towards the center of the visual field. If you start experiencing this symptom, you must attend to an emergency department right away.
8. Vision Loss
It is estimated that approximately 4.2 million Americans (40 years of age or older) are blind or have low vision1Common Eye Disorders and Diseases. (2020, June 03). Retrieved December 16, 2020, from https://www.cdc.gov/visionhealth/basics/ced/index.html. There are many possible causes of low vision and blindness, including retinal detachment. However, the leading causes of blindness in the US are other age-related diseases (age-related macular degeneration, diabetic neuropathy, cataract, and glaucoma).
As previously mentioned, a detached retina is a time-sensitive medical emergency because it can cause permanent blindness if untreated. When any section of the retina is detached from its normal position, it will cause some degree of vision loss. Fortunately, nowadays, surgical treatment for retinal detachment is usually successful; however, in some cases, vision may never fully return after surgery. The longer the detachment has been present and the more severe it is; the less vision can be expected to return. Similarly, people who have experienced several previous retinal detachments (chronic retinal detachment) are less likely to recover full vision after surgery.
9. Signs of Ocular Trauma
Recall that an important cause of retinal detachment (RD), especially in young people, is ocular trauma. In fact, the complications that result from this type of trauma are the most common cause of blindness (in one eye) in young people2Pitcher, J., MD. (2017, July 01). Traumatic Retinal Detachment in Younger Patients. Retrieved December 16, 2020, from https://www.retinalphysician.com/issues/2017/july august-2017/traumatic-retinal-detachment-in-younger-patients. One of these complications is retinal detachment, and it represents roughly 3 to 6 percent of all causes of this condition in children2Pitcher, J., MD. (2017, July 01). Traumatic Retinal Detachment in Younger Patients. Retrieved December 16, 2020, from https://www.retinalphysician.com/issues/2017/july august-2017/traumatic-retinal-detachment-in-younger-patients.
Given the possibility of RD after ocular trauma, when a person reports any of the possible symptoms of retinal detachment, the physician must always inquire about a history of trauma and check for possible signs of ocular trauma (cuts, bruises, eye redness, etc.). This is standard procedure because symptoms of RD can either occur immediately after the trauma or appear several days or months after the event.
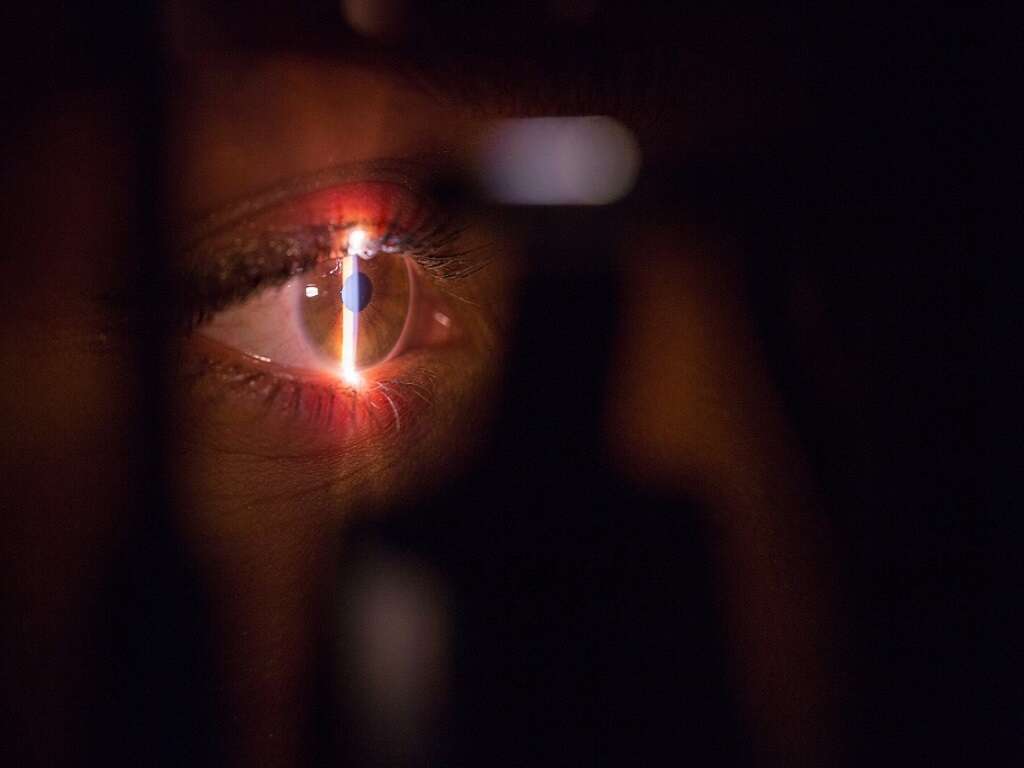
10. Abnormal Pupillary Response
The pupil is the black opening in the center of the eye. Its function is to allow the light to enter and focus on the retina. Moreover, both pupils are controlled by specific nerves and muscles that constrict them when the eye is focused on near objects or as a response to light. Conversely, these muscles work to dilate them in opposite situations. Pupillary response to light is usually consensual, which means that there will also be a change in the pupil size of the eye opposite to the one to which light is directed. This response is known as the pupillary light reflex and is usually evaluated through the swinging flashlight test.
Retinal detachment can cause abnormal pupillary responses. Specifically, it can cause a rare effect known as the Marcus Gunn pupil, where each pupil responds differently to light. For instance, the affected eye’s pupil will not constrict when light is shone during the swinging flashlight test. Yet, it will react when light is shone in the other eye. In short, the Marcus Gunn pupil indicates that there is a dysfunction in the retina (i.e. retinal detachment) or the optic nerve.